Health Conditions
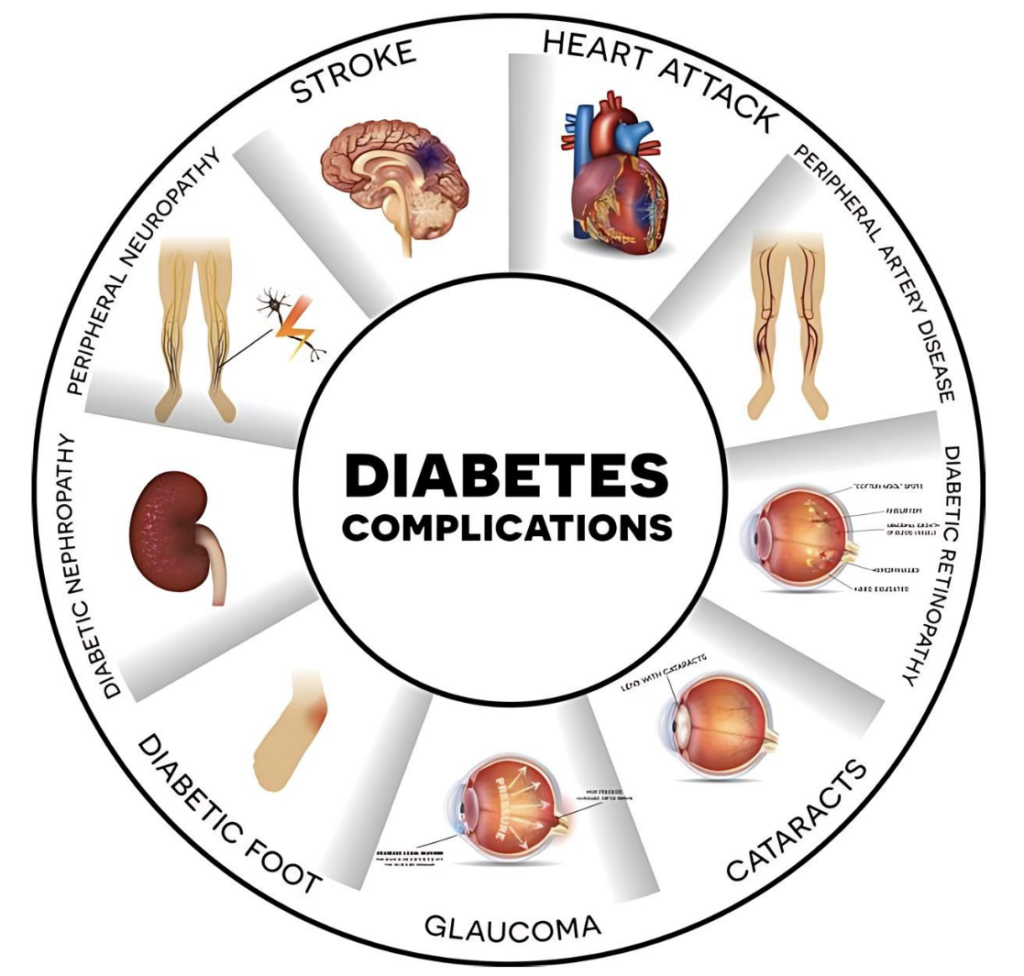
What are the Complications of Diabetes?
Elevated blood sugar levels are a serious hazard to overall health, especially in susceptible areas like the feet and eyes. These manifestations, known as diabetes complications, encompass a wide range of conditions that can have a significant impact on quality of life.
Despite this gloomy picture, there is one ray of hope: many of these diabetes complications are preventable. These consequences can be avoided or delayed via proactive management and lifestyle modifications, providing a route to improved well-being and longevity for diabetics.
Heart Disease
This is one of the most common complications that can happen to people with diabetes. Your doctor’s visits are meant to check for heart disease and help you stay away from major heart problems. They may do a number of tests during these visits, they will measure your blood pressure at every visit by putting a cuff around your upper arm that gets tighter as they measure how much blood is flowing through your arteries. Not only that, but they will also take a small amount of blood from your arm to check your triglyceride and LDL cholesterol readings.

An electrocardiogram at the start of the treatment plan is needed to finish the medical record. Learn more about the things that put you at risk for heart disease, like a family history of the disease or smoking.
Then, come up with a plan to stop it. For example, you could lose weight, start exercising regularly, learn how to deal with stress, and make sure that your blood pressure, cholesterol, and triglyceride levels stay within normal ranges.
Complications of Diabetes: Deep Dive on Cardiovascular Disease
Atherosclerosis
Diabetes hastens the progression of atherosclerosis, which causes arteries to constrict and harden as plaque accumulates. This syndrome reduces blood flow to essential organs like the heart, brain, and legs, raising the risk of heart attacks, strokes, and peripheral artery disease.
Coronary Artery Disease (CAD)
Diabetes increases the chance of developing coronary artery disease (CAD), a condition in which the coronary arteries that feed blood to the heart muscle narrow or become clogged due to plaque buildup. This can cause angina (chest pain) and, in severe situations, heart attacks.
Hypertension
People with diabetes are more likely to develop hypertension, which puts additional strain on the heart and blood vessels, raising the risk of cardiovascular problems.
Heart Failure
Diabetes raises the risk of heart failure, a condition in which the heart is unable to pump enough blood to fulfill the body’s needs. This can occur as a result of long-term hypertension, coronary artery disease, or cardiac muscle damage caused by diabetes problems.
Peripheral Artery Disease (PAD)
Diabetes leads to the development of PAD, which is characterized by constricted arteries in the legs that reduce blood flow to the extremities. PAD can cause discomfort, poor wound healing, infections, and, in extreme cases, gangrene and limb amputation.
Stroke
Diabetes increases the risk of stroke by increasing atherosclerosis and damaging blood vessels in the brain. Diabetes patients are more likely to have ischemic (blood clot) and hemorrhagic strokes.
Arrhythmias
Diabetes can disturb the heart’s normal electrical activity, resulting in arrhythmias such as atrial fibrillation and ventricular tachycardia. These irregular cardiac rhythms can raise the risk of a stroke or heart failure.
Endothelial Dysfunction
Diabetes compromises the function of the endothelium, or inner lining of blood vessels, resulting in endothelial dysfunction. This dysfunction contributes to the development and progression of cardiovascular disease by increasing inflammation, vasoconstriction, and irregular blood clotting.
Dyslipidemia
Diabetes frequently causes aberrant lipid profiles, including high levels of triglycerides, low levels of HDL cholesterol (the “good” cholesterol), and elevated levels of small, dense LDL particles. These lipid abnormalities lead to the progression of atherosclerosis and cardiovascular disease.
Microvascular Complications
While primarily affecting small blood vessels, diabetic retinopathy (affecting the eyes), diabetic nephropathy (affecting the kidneys), and diabetic neuropathy (affecting the nerves) can all indirectly contribute to cardiovascular disease by exacerbating hypertension and metabolic abnormalities.
Diabetic Nephropathy (Kidney Damage)
The kidneys are filtration miracles, diligently sifting through about half a cup of blood per minute to rid the body of metabolic waste and excess fluid. However, a dark threat lurks in the complex interplay between diabetes and renal health: the steady deterioration of renal function.
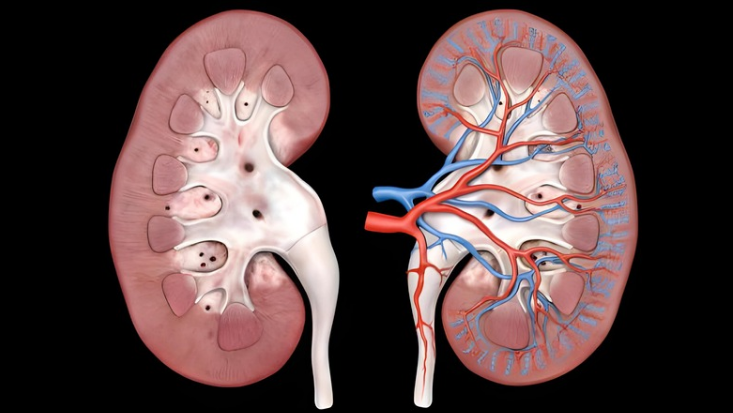
Over time, untreated diabetes can cause irreversible damage to these important organs, impairing their ability to filter waste items from the bloodstream. What are the consequences? Kidney insufficiency or failure necessitates immediate intervention, such as dialysis or kidney transplantation.
If you have a family history of kidney failure, high blood pressure, or heart disease, you may require more frequent testing. Some of these tests are:
- Albumin Test: Albumin is a blood protein that can be detected in urine if your kidneys are damaged. Your doctor will test a sample of your urine to see if albumin is present.
- GFR: A blood sample will also be collected to determine your glomerular filtration rate (GFR), which is a measure of how effectively your kidneys eliminate waste from your blood.
- Blood Pressure: Your physician will also check your blood pressure on a regular basis, as managing high blood pressure is vital in delaying the progression of kidney disease. Your reading should be lower than 130/80.
- Urinary Exam: If you have diabetes, you should get your urine tested once a year to see if you have diabetic nephropathy (also known as kidney disease).
- Creatinine: It is suggested that you have a baseline creatinine blood test to assess the function of your kidneys.
Diabetic Neuropathy (Nerve Damage)
As diabetes progresses, it can instigate nerve damage, a condition termed neuropathy, which manifests in a spectrum of symptoms including numbness, tingling, burning sensations, or outright pain in the hands, feet, or legs.

The emergence of these symptoms poses a significant concern as the numbness associated with neuropathy may obscure the perception of minor injuries, potentially allowing them to evolve into more serious complications over time.
To avoid future problems, check your feet and hands daily for symptoms:
- redness
- calluses
- cracks
- skin disintegration.
If you develop any of these symptoms between scheduled appointments, notify your healthcare professional right away.
Your healthcare practitioner may include or request particular diagnostic tests aimed at detecting diabetic neuropathy, such as:
Filament Testing
This entails using a specialized filament to assess feeling in different parts of the body, particularly the feet. If you can’t feel the filament’s touch in specific regions, this could suggest nerve damage.
Sensory Testing
This evaluates the response to stimuli such as heat, cold, or pressure, which aids in determining the extent of nerve damage and identifying afflicted areas.
Nerve Conduction Testing
This test determines the speed and strength of electrical signals as they flow via nerves. It can provide vital information on the extent of nerve injury and the specific nerves affected.
Electromyography (EMG)
This measures the electrical activity of muscles in response to nerve stimulation. This test helps to discover nerve dysfunction and differentiate between different types of neuropathy by examining muscle responses.
Autonomic Testing
This assesses the function of the autonomic nerve system, which regulates involuntary body functions like heart rate, digestion, and perspiration. Abnormal results may indicate autonomic neuropathy, a frequent consequence of diabetes that affects multiple organs and systems.
These specialist tests supplement the clinical evaluation, allowing for a more comprehensive assessment of diabetic neuropathy and specific treatment methods to manage symptoms and avoid consequences.
Diabetic Retinopathy (Eye Damage)
For people with diabetes, protecting their eyesight is very important. This means that they need to see an ophthalmologist (a specialist in eyes) at least once a year. An ophthalmologist uses a variety of diagnostic tools and techniques during these thorough eye exams to check the health of your eyes and look for any signs of diabetic retinopathy, a major problem with the retina that can happen because of diabetes.
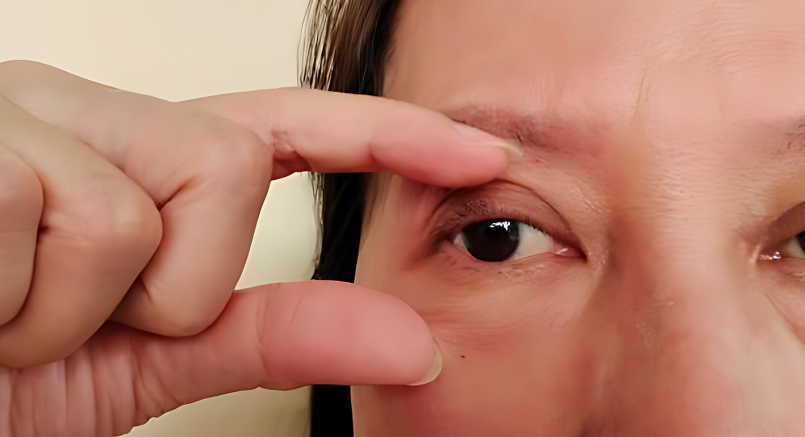
Eye drops that briefly make your pupils bigger are used to dilate your pupils, which is an important part of the exam. This lets the optician do a full check of the retina and optic nerves, which lets them find any problems or damage caused by diabetes. With the help of a special focusing lens, they carefully look at the retina’s complex structures, looking for signs of retinopathy like microaneurysms, bleeding, or swelling.
In addition to checking the retina, the ophthalmologist does other tests to get a better idea of your eyes’ general health and function. This includes checking your eye pressure to look for conditions like glaucoma, checking your side vision, and checking your farsightedness to make sure you have the best vision possible.
The eye exam is very important for finding and treating diabetic retinopathy early because it includes so many different tests. You can start treatments right away and keep your valuable sight.
Types of Diabetic Retinopathy
Early Diabetic Retinopathy
In this more prevalent variant, known as nonproliferative diabetic retinopathy (NPDR), new blood vessels do not sprout (proliferate).
Nonproliferative diabetic retinopathy (NPDR) causes the blood vessel walls in your retina to deteriorate. Small bulges emerge from the walls of smaller vessels, occasionally seeping fluid and blood into the retina. Larger retinal vessels may dilate and become uneven in diameter. NPDR can evolve from mild to severe as more blood vessels are blocked.
Sometimes retinal blood vessel injury causes an accumulation of fluid (edema) in the retina’s central section (macula). If macular edema impairs vision, therapy is necessary to avoid permanent vision loss.
Advanced Diabetic Retinopathy
Diabetic retinopathy can proceed to the more severe form, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close, resulting in the formation of new, aberrant blood vessels in the retina. These new blood vessels are delicate and may bleed into the clear, jellylike material that fills the center of your eye (vitreous).
Scar tissue formed by the formation of new blood vessels might eventually cause the retina to detach from the back of the eye. If the new blood vessels block the usual flow of fluid out of the eye, pressure can build up in the eyeball. This buildup can harm the optic nerve, which transmits images from your eye to your brain, resulting in glaucoma.
Foot Problems
Diabetes sufferers frequently experience foot complications. They can develop over time when high blood sugar levels harm the nerves and blood vessels in the feet. Diabetic neuropathy can cause numbness, tingling, discomfort, or lack of sensation in the foot.

If you are unable to feel discomfort, you may be unaware of a cut, blister, or ulcer on your foot. A wound like this could become infected. The infection may not heal properly because the damaged blood vessels can result in inadequate blood flow in your foot.
Infection and inadequate blood flow can cause gangrene. This means that muscles, skin, and other tissues begin to perish. If gangrene or a foot ulcer persists despite therapy, amputation may be necessary. This is a surgical procedure that removes your damaged toe, foot, or leg. It may keep a serious illness from spreading and possibly save your life.
However, there is a lot you can do to keep a foot wound from becoming a serious health issue.
Prevention
The greatest strategy to preserve your feet is to maintain healthy blood sugar levels on a daily basis. This will assist in preventing further nerve and blood vessel damage. The second step is to keep the skin on your feet healthy.
Good foot care for diabetics includes:
- Check your feet every day. Look for wounds, redness, and other changes in the skin and toenails, such as warts or other areas where your shoes may rub. Also, make sure to inspect the bottoms of your feet.
- Wash your feet every day. Use warm water and soap. Don’t wet your feet because it can cause your skin to dry out. After you’ve dried your feet, apply talcum powder or cornstarch between your toes. They absorb moisture, which can cause infection. If you use lotion, avoid applying it between your toes.
- Consult your doctor about safe methods for removing corns and calluses. Thick skin on your foot can rub and cause ulcers. However, removing it incorrectly can cause damage to your skin. So avoid cutting the skin and using medicated pads or liquid removers.
- Trim your toenails straight across with a clipper. If you find it difficult to trim your own toenails, or if they are thick or curl into the skin, hire a podiatrist (foot doctor).
- Always wear well-fitting shoes, socks, or slippers to protect your feet while walking. You do not want to walk barefoot, even indoors. Make sure your shoes are smooth inside. A seam or stone could scrape your flesh raw.
- Protecting your feet from the heat and cold. Use sunscreen on exposed skin and avoid walking barefoot on the beach. In cold weather, wear warm socks instead of putting your feet near a heater or fireplace.
- Keeping blood circulating via your feet. Sit with your feet up. Wiggle your toes and circle your feet all day. Do not wear tight socks. Get lots of activities that aren’t too strenuous on your feet, like walking.
- Have your feet checked at your healthcare appointments. Even if you haven’t observed any problems, it’s a good idea to have your doctor examine your feet.
Skin Problems

There are a variety of diseases and conditions that can affect your skin. Some may produce unpleasant feelings such as itching, burning, redness, and rashes. They may also affect your physical appearance. Some of the most common skin conditions are:
Acne
Acne can be more severe in diabetics because of poor circulation and elevated blood sugar levels, which can aggravate inflammation and slow the healing process of clogged hair follicles. High blood sugar creates a favorable environment for bacterial development, complicating acne treatment.
Burns
Diabetes can affect the body’s capacity to heal wounds, making burns especially harmful because they can cause infections and slow recovery. Neuropathy, a common symptom of diabetes, can also cause diminished sensitivity, making people less aware of tiny burns that could lead to more serious injuries.
Cuts and Scrapes
Cuts and scrapes are more likely to become infected and heal slowly in diabetics due to reduced immune function and poor blood circulation. This can result in persistent sores or ulcers, especially on the foot, requiring substantial medical attention.
Dandruff
Diabetes can dehydrate and oilify the skin, worsening dandruff. Poor blood sugar control can also cause fungal infections on the scalp, resulting in persistent peeling and discomfort.
Eczema (Atopic Dermatitis)
Diabetes can exacerbate eczema by reducing the skin’s capacity to absorb moisture, resulting in increased dryness, irritation, and susceptibility to infections. High blood sugar levels can irritate the skin and complicate eczema treatment.
Hives
Hives, also known as urticaria, might be more common and severe in diabetics due to an overactive immune system and increased inflammation. Additionally, certain diabetic drugs may cause allergic responses, resulting in hives.
Insect Bites
Insect bites can be especially problematic for diabetics because they cause more intense reactions, delayed recovery, and an increased risk of infection. Diabetes-related poor immune response and decreased circulation can exacerbate these problems.
Psoriasis
Psoriasis can be more severe in people with diabetes due to persistent inflammation and immune system dysfunction. Diabetes-related systemic inflammation can aggravate the frequency and severity of psoriasis flare-ups.
Skin Cancer
Diabetes may raise the risk of skin cancer because persistent high blood sugar levels weaken the immune system and impair the skin’s ability to repair DNA damage. Skin cancer risk management in diabetes people requires regular monitoring and early identification.
Skin Infections
Diabetes increases the risk of skin infections because high blood sugar levels damage the immune system, restrict blood flow, and provide an ideal habitat for bacterial and fungal growth. Common infections include cellulitis, fungal infections, and diabetic ulcers, all of which require fast and appropriate treatment to avoid complications.
Depression and Anxiety
Diabetes and Depression
Some symptoms of depression are similar to those of diabetes. Both conditions might cause you to be fatigued, sleep a lot, and have difficulties concentrating. This makes it difficult to determine if your symptoms are caused by depression, diabetes, or both.
Diabetics are twice as prone to experience depression.

Does Diabetes Lead to Depression?
Diabetes does not directly cause depression, although the disease’s complications and characteristics can contribute to its development. Dealing with the constant presence of this illness can be stressful, especially with additional decision-making responsibilities.
If you had depression before developing diabetes, it can exacerbate your depression.
Does Depression Cause Diabetes?
Previous research indicates that those with type 1 and type 2 diabetes are more likely to experience depression, and those with depression have a higher chance of getting type 2 diabetes. A Diabetes UK-funded study found that depression can directly increase the chance of getting type 2 diabetes. The study’s findings highlighted the impact of depression on increased body mass index (BMI) and suggested that this somewhat, but not entirely, explained the link between depression and diabetes. The study also identified seven genetic alterations that can contribute to depression and diabetes. The common genes influence how insulin is produced and can promote inflammation in the brain, pancreas, and fat tissues.
These changes in the body demonstrate how depression may increase the risk of type 2 diabetes. The association between depression and type 2 diabetes is complex, but this study sheds new light on the subject.
While studies have revealed that patients with type 1 diabetes may be more likely to suffer sadness, depression is not a risk factor.
A few symptoms of depression can have a direct impact on your diabetes management, such as:
- I don’t want to do anything or see anyone. You might not be managing your diabetes appropriately. This may include not taking medicine checking blood sugars, skipping doctor appointments, or neglecting health issues. All of them could cause difficulties.
- Feeling low frequently and for extended periods of time.
- Having difficulty getting out of bed or frequently waking up at night.
- Feeling tired more often than not. This could prevent you from exercising, which can improve your diabetes management.
- Overeating can lead to elevated blood sugar levels.
- Not eating enough can cause hypoglycemia, especially if taking insulin or other medications with this negative effect.
- Feeling self-conscious and anxious about disappointing loved ones.
- Difficulties with concentration and distractions.
- Feeling agitated and nervous.
- Moving slowly and reluctant to talk.
- Suicidal thoughts or feelings of wanting to die. Depression can also cause self-destructive behavior, and if you believe you’d be better off dead, you may cease caring for yourself.
Complications During Pregnancy
Gestational diabetes can significantly increase the risk of complications for both the mother and the baby. For the mother, gestational diabetes can lead to conditions such as preeclampsia, a potentially dangerous increase in blood pressure, and a higher likelihood of requiring a cesarean section due to the baby’s larger size.

For the baby, the risks include premature birth, which can result in respiratory distress syndrome and other health issues associated with early delivery. Additionally, babies born to mothers with gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
Proper management and monitoring of blood sugar levels during pregnancy are crucial to minimize these risks and ensure the health and well-being of both mother and child.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
Sources Expanded
- B. (n.d.). Depression and diabetes. Diabetes UK. https://www.diabetes.org.uk/guide-to-diabetes/emotions/depression#:~:text=If%20you%20have%20diabetes%2C%20you,psychological%20wellbeing%20since%20being%20diagnosed.
- Diabetes Complications. (n.d.). MedlinePlus. https://medlineplus.gov/diabetescomplications.html
- Skin Conditions. (n.d.). Hives | Acne | MedlinePlus. https://medlineplus.gov/skinconditions.html
- Diabetic Foot. (n.d.). MedlinePlus. https://medlineplus.gov/diabeticfoot.html
- Lower Your Risk of Diabetes Complications | ADA. (n.d.). https://diabetes.org/about-diabetes/complications
- Diabetes Complications. (2024, March 15). WebMD. https://www.webmd.com/diabetes/diabetes-complications
- Society, E. (2023, January 4). Diabetes Complications. Endocrine Society. https://www.endocrine.org/patient-engagement/endocrine-library/diabetes-complications
Trusted Health, Wellness, and Medical advice for your well-being