Health Conditions
Effective Treatment Strategies for Whooping Cough
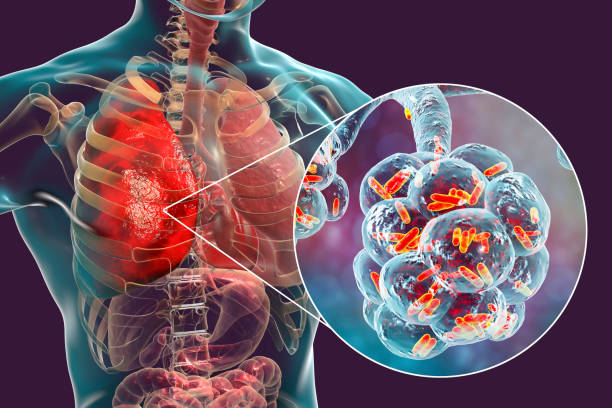
Whooping cough, caused by the Bordetella pertussis bacteria, is very contagious.
This illness, which causes severe coughing for weeks or months, is harmful to babies and young children. Vaccination protects against whooping cough, but infection is still possible; thus, immediate treatment is required to avoid complications.
Antibiotics minimize whooping cough symptoms, duration, and transmission. Early treatment, within two weeks of symptom onset, is critical, with hospitalization recommended for vulnerable populations such as babies and people with underlying health problems.
Antibiotics are only one of many symptom management and rehabilitation strategies. Rest, drink, and a reduction in smoke and dust are critical. Under physician supervision, over-the-counter cough suppressants and pain relievers may give symptomatic relief.
Understanding whooping cough management is vital for navigating its complexities. We can tackle this infectious disease and improve outcomes for individuals and communities by introducing early treatment and comprehensive care.
Understanding Whooping Cough
Whooping cough, or pertussis, is a highly contagious bacterial infection caused by Bordetella pertussis. It is distinguished by intense coughing bouts that might last many weeks and are sometimes accompanied by a whooping sound when the sufferer attempts to inhale.
Causes and Transmission
When an infected individual coughs or sneezes, the bacteria responsible for whooping cough spread through the air. The disease is very contagious and quickly passed from person to person, particularly in crowded environments like schools and daycare centers.
Signs and Symptoms
Whooping cough symptoms typically include a runny nose, sneezing, and a slight cough. After a week or two, the cough worsens and may be followed by vomiting and tiredness. In extreme circumstances, the coughing bouts are so intense that the sufferer turns blue or vomits blood.
Diagnosis Methods
Diagnosing whooping cough can be challenging because its early symptoms resemble those of a normal cold. Doctors may consider whooping cough if a patient has a chronic cough for more than two weeks and makes a whooping sound. To confirm the diagnosis, doctors may request a blood test, a nasal or throat swab, or a chest x-ray.
If you suspect you or your kid have whooping cough, seek medical assistance right once. Early identification and treatment can help prevent complications and slow the spread of the disease.

Medical Treatment Options for Whooping Cough
There are several medical treatment options for whooping cough. The two primary alternatives are antibiotics and hospitalization and monitoring.
Antibiotics and Prescriptions
If a patient is diagnosed with whooping cough, their doctor may prescribe medications to treat the condition. Antibiotics can help minimize the duration of the sickness and the intensity of the symptoms. The most common antibiotics recommended for whooping cough are azithromycin, erythromycin, and clarithromycin.
It’s vital to remember that antibiotics are only helpful if given early in the illness. If someone has been unwell for more than three weeks, antibiotics may be less effective at treating the infection.
Hospital Care and Monitoring
In severe cases of whooping cough, hospitalization may be required. Hospital care can help you control your symptoms and avoid problems. Hospital treatment for whooping cough often focuses on keeping breathing passages clear, monitoring breathing and administering oxygen as needed, and preventing or treating dehydration.
If someone is hospitalized for whooping cough, they may require intravenous (IV) fluids if they appear dehydrated or have difficulties eating. Hospital treatment and monitoring can assist to avoid significant problems and guarantee a complete recovery.
Overall, it is critical to get medical attention if you feel you or someone you know has whooping cough. Antibiotics and hospitalization can help alleviate symptoms and prevent complications.

Home Care and Management
Hydration and Nutrition
One of the most critical components of home care for whooping cough is keeping the patient hydrated and well-fed. Drinking plenty of fluids is critical in preventing dehydration, especially if the patient is vomiting or has diarrhea. Small, regular meals throughout the day can help you stay energized and avoid nausea. It is advised to avoid heavy meals because they can cause coughing fits.
Environment and Comfort
Creating a warm and calming environment might help relieve the symptoms of whooping cough. Rest is necessary for the body to recuperate, so avoid strenuous activity and get plenty of sleep. A cool, dark, and quiet bedroom might help a patient relax and sleep better. A humidifier can also help keep the air moist and reduce coughing episodes. Suctioning mucus from the nose and throat can also improve breathing and prevent problems.
It is crucial to understand that cough treatment, including over-the-counter cough drugs, is not advised for treating whooping cough. These drugs can aggravate the cough and prolong the illness. If the symptoms are severe or the patient has experience.

Prevention and Vaccination for Whooping Cough
Whooping Cough Vaccination
The most effective way to avoid whooping cough (pertussis) is by vaccination. Pertussis vaccines are typically administered in conjunction with diphtheria and tetanus vaccines (DTaP or Tdap). The vaccine is indicated for newborns, children, and adults.
Infants should receive the DTaP vaccination at two, four, and six months of age, with booster shots at 15-18 months and 4-6 years of age. To protect their newborns, adults should receive the Tdap vaccine once, while pregnant women should receive it throughout each pregnancy.
The vaccine is safe and effective, with very few major adverse effects. Mild side effects may include soreness, redness, or swelling at the injection site, as well as fever, headache, or exhaustion.
Protecting Infants and High-Risk Groups
Infants and young children are most susceptible to severe complications from whooping cough, including hospitalization and death. Pregnant women, persons with compromised immune systems, and those with certain medical disorders are all at higher risk.
To protect babies and high-risk groups, everyone should receive the pertussis vaccine. This includes parents, caregivers, and healthcare staff who may interact with infants.
If someone in your household has whooping cough, you should take precautions to prevent the disease from spreading. This includes staying home from school or work, covering coughs and sneezes, and washing your hands frequently.
Furthermore, if someone is diagnosed with whooping cough, medications may be prescribed for close contacts in order to prevent the disease from spreading. This is especially crucial for people who are at a higher risk of serious problems.
Conclusion
In conclusion, we must remain committed to finding treatment strategies for whooping cough. After studying this highly contagious respiratory infection’s insidious nature, it’s evident that everyone is vulnerable, especially the most vulnerable.
However, with vaccine and antibiotic therapy, we can defeat whooping cough. We can reduce this disease’s terrible effects by promoting widespread immunization, early intervention, and comprehensive symptom management.
Our efforts must continue. Whooping cough prevention requires education, awareness, and community engagement. We must work together to end coughing spells and protect everyone from contagious diseases.
Let us persevere to abolish whooping cough. Working together can reduce coughing spells and secure a healthy future for future generations.
Trusted Health, Wellness, and Medical advice for your well-being


