Health Conditions
How Liver Fibrosis Is Quietly Damaging Your Health
The excessive buildup of scar tissue in the liver is a characteristic of the degenerative illness known as hepatic fibrosis. It is a reaction to persistent liver damage brought on by liver disorders other than non-alcoholic fatty liver disease (NAFLD), viral hepatitis, alcohol misuse, or other underlying liver injuries. If treatment is not received, liver tissue scarring can deteriorate liver function and cause major problems.
As the liver tries to heal itself in reaction to continuous injury, fibrosis develops. Scar tissue can eventually distort the liver’s natural shape, making it more difficult for the organ to carry out crucial processes including metabolic regulation, production of necessary proteins, and removal of toxins from the blood.
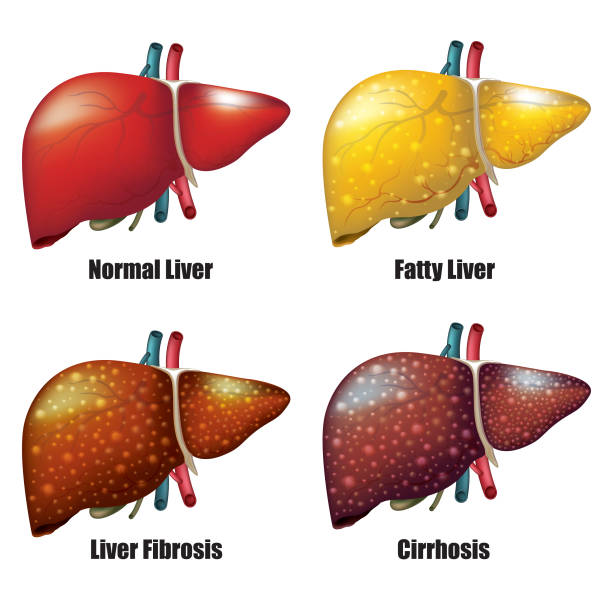
Liver fibrosis can proceed slowly; in its early stages, it frequently shows no symptoms at all. But when the illness worsens, it can cause a major impairment in liver function and raise the chance of developing more serious liver conditions including liver cancer and cirrhosis.
Causes and Risk Factors for Liver Fibrosis
Liver fibrosis can arise due to a multitude of circumstances. Because alcohol may directly harm liver cells and promote inflammation and scarring, it is one of the main causes of liver fibrosis. If left untreated, viral infections—especially hepatitis B and C—can also result in chronic liver damage and inflammation. Furthermore, a prominent cause of liver fibrosis is non-alcoholic fatty liver disease (NAFLD), which is defined by the buildup of fat in the liver, particularly in those who have metabolic syndrome and obesity.
Additional risk factors for liver fibrosis include exposure to certain chemicals or medicines, autoimmune liver illnesses, genetic abnormalities affecting liver function, and conditions like primary biliary cholangitis that cause disruptions in bile flow. Effectively managing or preventing liver fibrosis requires an awareness of these risk factors and taking appropriate action.
Symptoms and Signs of Liver Fibrosis
Liver fibrosis may not exhibit any symptoms in its early stages, making a diagnosis difficult without certain medical testing. People may develop symptoms including weakness, exhaustion, unexplained weight loss, and upper right abdominal pain as the illness worsens. It’s crucial to remember that these symptoms can also be linked to other medical disorders, which emphasizes the necessity of a thorough medical examination and testing to identify liver fibrosis.
Liver fibrosis can occasionally present as liver function-related problems such jaundice, leg or abdominal edema, and easily bruising or bleeding. These symptoms point to more severe liver injury and need for immediate medical intervention.
Diagnosis and Staging of Liver Fibrosis
A combination of imaging scans, physical examinations, laboratory testing, and medical history evaluation is usually used to diagnose liver fibrosis. Imaging methods including magnetic resonance imaging (MRI), computed tomography (CT) scans, and ultrasound may offer comprehensive pictures of the liver, which can be used to measure the amount of liver damage and spot fibrosis symptoms.
Additionally, blood tests are essential for assessing liver function and identifying certain fibrosis indicators, such as aberrant protein levels, raised liver enzyme levels, and the presence of chemicals linked to fibrosis in the blood. A liver biopsy may be suggested in specific circumstances in order to collect a tissue sample for accurate hepatic fibrosis staging and to inform therapy choices.
Complications of Advanced Liver Fibrosis
When liver fibrosis reaches more advanced stages, serious consequences may arise that have a substantial negative influence on general health. Life-threatening consequences such as portal hypertension, liver failure, and an elevated risk of liver cancer can arise from cirrhosis, a late stage of liver fibrosis marked by extensive scarring and liver malfunction.
Varices, or bulging veins, can occur in the gastrointestinal system and are prone to bleeding. Portal hypertension is brought on by an increase in pressure in the portal vein. Furthermore, decreased liver function might have an impact on blood coagulation, which raises the possibility of bleeding and makes bruising easier. Knowing the possible side effects of advanced liver fibrosis highlights the significance of continuing care and early intervention.
Treatment Options for Liver Fibrosis
The goals of liver fibrosis treatment are to delay or stop the disease’s progression, cure the underlying source of liver damage, and stop the development of more serious liver illnesses. Giving up alcohol is crucial for those with alcoholic liver disease in order to stop more liver damage from occurring and to encourage liver regeneration. Similar to that, antiviral medication can effectively control viral hepatitis and slow the advancement of liver fibrosis and inflammation.
Lifestyle changes, including as losing weight, eating a balanced diet, and engaging in regular exercise, are essential for controlling non-alcoholic fatty liver disease and halting the advancement of fibrosis. In certain instances, drugs that target certain pathways involved in the formation of fibrosis may be administered in an effort to enhance liver function and slow down the scarring process.
In patients with severe liver cirrhosis or fibrosis, liver transplantation can be the only effective course of treatment. With this surgical technique, there is a possibility for better long-term results and quality of life when the diseased liver is replaced with a healthy donor liver.

Lifestyle Changes to Manage Liver Fibrosis
Adopting good lifestyle choices can assist people with liver fibrosis better control their illness and enhance overall liver health in addition to medication therapies. Lean protein, whole grains, fruits, and vegetables are high in balance and can help promote liver function and prevent the buildup of fat in the liver.
Frequent exercise can help manage liver fibrosis by promoting weight control, enhancing insulin sensitivity, and lowering the risk of the advancement of fatty liver disease. Limiting exposure to toxins and hazardous chemicals and abstaining from excessive alcohol intake are crucial measures in halting more liver damage and promoting liver regeneration.
Additionally, people who have liver fibrosis should make routine checkups a priority, follow their doctors’ orders, and look for help from medical experts and support groups for any difficulties relating to their disease.
Diet and Nutrition for Liver Health
The key to maintaining liver function and controlling liver fibrosis is eating a balanced diet. Particular nutrients and dietary elements can help lower inflammation, encourage liver regeneration, and stop liver fibrosis from progressing. Adequate use of antioxidants, including vitamin C, vitamin E, and selenium, can lessen the likelihood of fibrosis formation and shield liver cells from oxidative stress.
Furthermore, it has been demonstrated that foods high in omega-3 fatty acids, such walnuts, flaxseeds, and fatty fish, have anti-inflammatory properties and may help those who have liver fibrosis. Reducing the consumption of processed foods, refined sugars, and saturated fats is crucial to avoiding liver fat formation and lowering the chance of worsening hepatic fibrosis.
It’s critical that people with liver fibrosis collaborate with a medical expert or registered dietitian to create a customized nutrition plan that satisfies their unique dietary requirements and promotes optimal liver function.
Support and Resources for Individuals with Liver Fibrosis
Living with liver fibrosis can come with a number of psychological and physical difficulties. It is crucial for people with liver fibrosis to look for assistance and make use of services that might help them manage their illness. For people and their families, support groups, internet forums, and neighborhood organizations devoted to liver health can offer helpful knowledge, direction, and a feeling of community.
Furthermore, the involvement of healthcare providers is critical in providing patients with liver fibrosis with comprehensive treatment and management techniques. These providers include gastroenterologists, hepatologists, and specialist liver clinics. These specialists can provide individualized treatment regimens, consistent monitoring, and advice on lifestyle adjustments to improve liver function and lessen the symptoms of fibrosis.
Individuals with liver fibrosis can also be empowered to take an active role in their health and contribute to ongoing efforts to improve liver fibrosis outcomes by having access to credible educational materials, keeping up to date on developments in the management of liver disease, and taking part in clinical trials or research studies.
Conclusion
The journey to optimal liver health is a vital aspect of overall well-being, and understanding the risks and signs of liver fibrosis is crucial. As we unravel the complexities of our bodies, it becomes evident that proactive measures are the key to maintaining a healthy liver. Remember, a balanced lifestyle, regular exercise, and a mindful approach to nutrition can go a long way in preventing and managing liver fibrosis. Listen to your body, prioritize your health, and consult with healthcare professionals for personalized guidance. Let’s embark on a path of liver wellness, ensuring that our bodies function at their best for a vibrant and fulfilling life.

