Health Conditions, Reproductive Health
Traditional Methods Of Syphilis Diagnosis
Syphilis, a sexually transmitted infection caused by the bacteria Treponema pallidum, has afflicted humans for ages. Long before modern laboratory techniques, physicians used a range of conventional methods to identify this mysterious condition. This article delves into the historical procedures and techniques used to diagnose syphilis before to the introduction of modern medicine. From symptom monitoring and physical examination to the use of antique diagnostic equipment, we explore the intriguing history of syphilis identification and diagnosis. Join us on a journey back in time to discover the old approaches that shaped our understanding and diagnosis of this difficult sickness.
Historical Overview of Syphilis Diagnosis
Development of Serologic Tests
The development of serologic assays for syphilis diagnosis began in the early twentieth century. August von Wassermann created the first test, known as the Wassermann test, in 1906. This test employed the complement fixation principle to detect antibodies to the syphilis-causing bacteria Treponema pallidum.
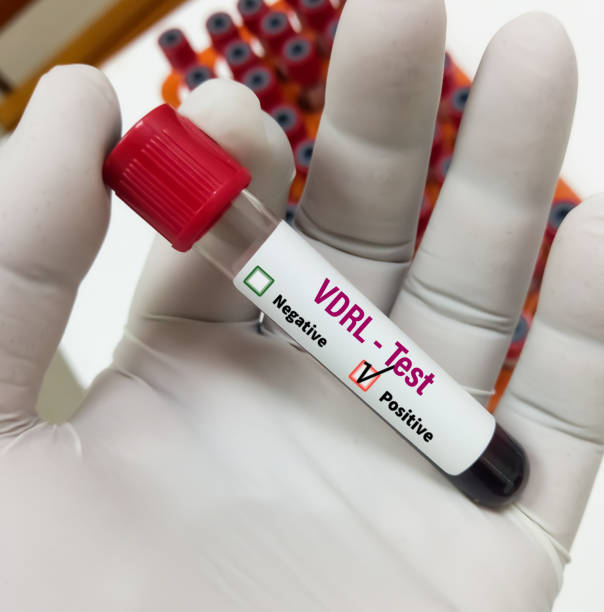
In 1946, the Venereal Disease Research Laboratory (VDRL) test was introduced. This test was a variation on the Wassermann test and was used to identify antibodies to lipids produced by injured host cells. The VDRL test was widely used for many years, however it has drawbacks, such as false-positive results caused by cross-reactivity with other disorders.
The rapid plasma reagin (RPR) test was developed in the 1970s. This test outperformed the VDRL test in terms of sensitivity and specificity. The RPR test used the same premise as the VDRL test, but with a different antigen preparation.
Evolution of Diagnostic Algorithms
Over time, syphilis diagnosis algorithms have evolved. Previously, syphilis was diagnosed using a mix of clinical signs and symptoms, such as the formation of a chancre or rash, as well as laboratory tests.
Today, syphilis is diagnosed using a mix of scientific tests and clinical examination. The Centers for Disease Control and Prevention (CDC) recommends a two-step syphilis test. The initial step is to administer a nontreponemal test, such as the RPR or VDRL test. If this test yields a positive result, a confirmatory treponemal test, such as the fluorescent treponemal antibody absorption (FTA-ABS) or the Treponema pallidum particle agglutination (TP-PA) test, should be conducted.
To summarize, the introduction of serologic tests and the evolution of diagnostic algorithms have significantly enhanced the accuracy and reliability of syphilis diagnosis. The CDC-recommended two-step technique is now widely regarded as the gold standard for syphilis testing.
Non-Treponemal Tests for Syphilis
Non-treponemal tests are the most usually employed to diagnose syphilis. These tests detect the host’s antibodies to the lipoidal material generated by injured host cells as a result of Treponema pallidum infection. The Venereal Disease Research Laboratory (VDRL) test and the Rapid Plasma Reagin (RPR) test are the two most popular non-treponemal tests.
Venereal Disease Research Laboratory Test
The VDRL test is a simple, quick, and inexpensive method for detecting the presence of nontreponemal antibodies in the patient’s serum or plasma. The test works on the idea of flocculation, in which the antigen-antibody combination creates visible clumps that may be seen under a microscope. The VDRL test is used to detect syphilis and monitor treatment efficacy. However, the test is not specific to syphilis and may produce false-positive results in patients with lupus, malaria, or leprosy.
Rapid Plasma Reagin Test
The RPR test is another prominent nontreponemal test for syphilis diagnosis. The test operates on the concept of cardiolipin antigen, which is coated on the surface of carbon particles. The test reveals the presence of non-treponemal antibodies in the patient’s serum or plasma. The RPR test is more sensitive than the VDRL test and can detect infections in their early stages. However, the test can produce false-positive results in persons with other disorders such lupus, malaria, and leprosy.
Finally, non-treponemal assays such as VDRL and RPR are widely utilized in the diagnosis of syphilis. These tests are easy, fast, and inexpensive, but they are not specific to syphilis and may produce false-positive results in people with other disorders. To accurately diagnose syphilis, these tests should be used in conjunction with treponemal assays.
Treponemal Tests for Specific Antibody Detection
The standard approach for diagnosing syphilis consists of two steps: a nontreponemal test, followed by a treponemal test for confirmation. Treponemal assays detect particular antibodies to T. pallidum and are more specific than nontreponemal testing.
Fluorescent Treponemal Antibody Absorbed Test
The Fluorescent Treponemal Antibody Absorbed Test (FTA-ABS) detects particular treponemal antibodies by the use of fluorescently tagged antibodies. It is highly sensitive and specific, and is often regarded as the gold standard for syphilis diagnosis. However, performing the test requires specialized equipment and qualified workers.
T. Pallidum Particle Agglutination
The T. Pallidum Particle Agglutination (TPPA) test is another treponemal test that identifies antibodies to T. pallidum. It is a simple and dependable test that may be carried out in most clinical laboratories. Although less sensitive than FTA-ABS, it is nonetheless regarded as a highly specific test for the diagnosis of syphilis.
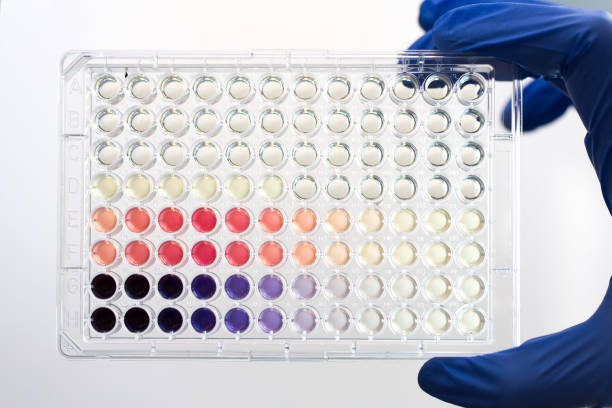
Enzyme Immunoassays
Enzyme Immunoassays (EIAs) are treponemal diagnostics that use enzymes to identify specific treponemal antibodies. They are simple to perform and may be automated, making them an attractive option for large-scale screening programs. They are less sensitive than FTA-ABS and TPPA, though, and may provide false-positive results in some circumstances.
In summary, treponemal assays detect particular antibodies to T. pallidum. FTA-ABS is considered the gold standard for diagnosing syphilis, while TPPA and EIAs are equally reliable tests that can be performed in most clinical laboratories. However, each test has advantages and limitations, and the choice of test is determined by the specific clinical circumstance.
Clinical Considerations in Syphilis Diagnosis
Treponema pallidum bacteria causes syphilis, a sexually transmitted ailment. If not treated, the infection might cause major health consequences. As a result, early identification and treatment are critical to avoiding consequences. Traditional syphilis diagnosis relies on serological tests that detect antibodies to T. pallidum in blood or other bodily fluids. However, there are some clinical factors to consider while diagnosing syphilis.
Neurosyphilis and Cerebrospinal Fluid Analysis
Neurosyphilis is a severe consequence of syphilis that affects the central nervous system. It can occur at any stage of syphilis, but it is most frequent in the late stages. Therefore, it is crucial to consider neurosyphilis in patients with late-stage syphilis or neurological symptoms. Cerebrospinal fluid (CSF) analysis is the gold standard for detecting neurosyphilis. A lumbar puncture is used to retrieve CSF, which is then analyzed for T. pallidum antibodies, cell count, protein, and glucose. A positive CSF test for T. pallidum antibodies suggests neurosyphilis, even if the blood test is negative.
Congenital Syphilis and Maternal Screening
Congenital syphilis is a dangerous disorder in which a pregnant woman with syphilis transmits the infection to her unborn child. The infection can result in stillbirth, preterm, poor birth weight, and a variety of other health complications. As a result, early detection and treatment of syphilis in pregnant women is critical to preventing congenital syphilis. The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) both suggest maternal screening for syphilis during pregnancy. The screening includes a blood test for syphilis antibodies. Pregnant women who test positive for syphilis should get penicillin to prevent transmission to the fetus. Infants born to moms with syphilis should be checked and treated right away to avoid problems.
Finally, clinical aspects are significant for diagnosing syphilis. Neurosyphilis should be considered by healthcare practitioners for people with late-stage syphilis or neurological symptoms. CSF analysis is considered the gold standard for diagnosing neurosyphilis. Pregnant women should be checked for syphilis to avoid congenital disease. Early detection and treatment of syphilis are critical for reducing complications and improving patient outcomes.
Conclusion
Finally, the historical voyage of syphilis diagnosis reveals an intriguing assortment of ancient methods that were used prior to the introduction of contemporary medical tools. Throughout history, conventional techniques to syphilis diagnosis and comprehension included observing symptoms and physical indicators as well as using archaic diagnostic tools. While these procedures may appear primitive by today’s standards, they set the groundwork for the development of current diagnostic tools and demonstrate the continued importance of clinical observation and empirical reasoning in medicine. As we reflect on the past, let us remember our forefathers’ inventiveness and determination in facing the problems of syphilis diagnosis and treatment, while also acknowledging the continuous advances that continue to impact our understanding and care of this complicated disease.
Trusted Health, Wellness, and Medical advice for your well-being


