Health Conditions
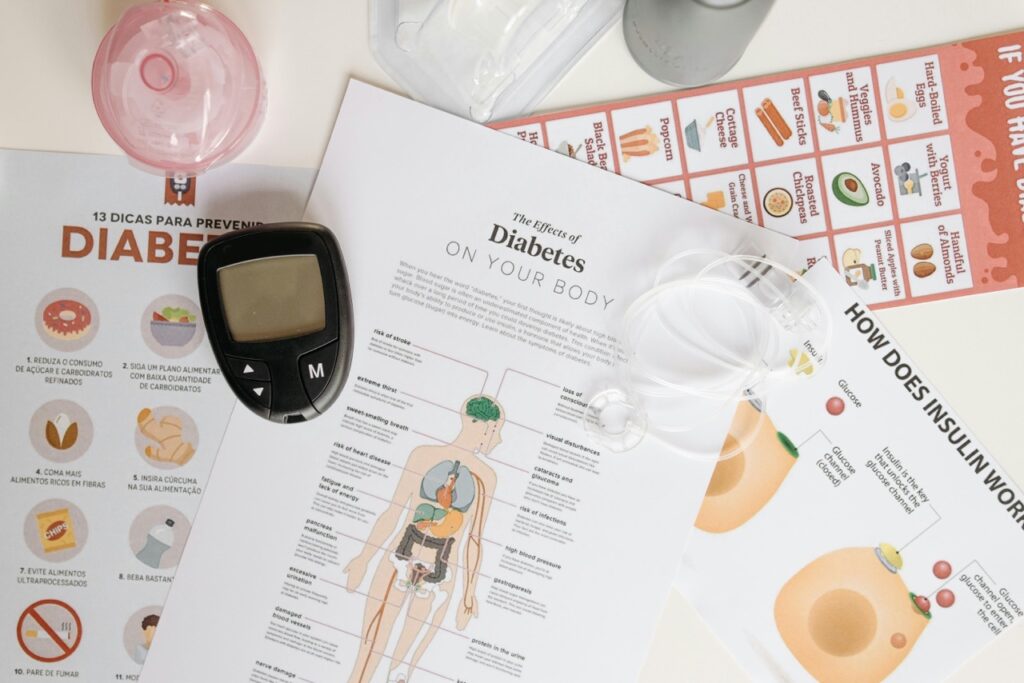
Understanding Diabetes as a Chronic Health Condition
Welcome to our article on understanding diabetes as a chronic health condition. With an estimated 463 million people worldwide living with diabetes, it is essential to shed light on this prevalent and potentially life-altering condition. In this article, we will go into the fundamental aspects of diabetes, including its causes, symptoms, and long-term effects on overall health.
We will also explore the different types of diabetes and provide practical tips for managing this chronic health condition effectively. Whether you are newly diagnosed or seeking to expand your knowledge, this guide aims to equip you with the necessary information to navigate life with diabetes. Let’s get started on the path to understanding and empowering ourselves in managing this chronic health condition.
Definition and Characteristics of Chronic Health Conditions
Chronic health conditions are distinguished by their prolonged duration and the requirement for continued medical care. These diseases usually develop slowly and deteriorate gradually. Chronic ailments, as opposed to acute disorders, are long-term and may necessitate ongoing management. Heart disease, asthma, arthritis, and diabetes are some common chronic health issues.
Living with a chronic ailment can be difficult because it typically necessitates considerable adjustments in lifestyle and daily activities. The impact of chronic diseases varies greatly depending on the condition and its severity. Some chronic diseases may cause little disturbance in a person’s life, but others may significantly limit their abilities and necessitate ongoing medical attention.

Types of Diabetes – Type 1 and Type 2
Diabetes is a chronic health condition that impairs the body’s capacity to control blood sugar levels. There are two forms of diabetes: type 1 and type 2.
Type 1 Diabetes
Type 1 diabetes, commonly known as insulin-dependent diabetes, is an autoimmune illness in which the body’s immune system incorrectly assaults and destroys insulin-producing cells in the pancreas. As a result, the body is unable to create sufficient insulin to regulate blood sugar levels adequately. Type 1 diabetes usually begins in infancy or adolescence, but it can occur at any age.
To keep blood sugar levels consistent, people with Type 1 diabetes must take insulin for the rest of their lives. They must closely monitor their blood glucose levels and deliver insulin via injection or an insulin pump. The proper management of Type 1 diabetes entails combining insulin doses with food intake, physical exercise, and other factors that can alter blood sugar levels.
Type 2 Diabetes
kind 2 diabetes is the most prevalent kind of diabetes, accounting for approximately 90% of all cases. Unlike Type 1 diabetes, Type 2 diabetes is distinguished by insulin resistance, which means that the cells in the body do not respond adequately to insulin’s effects. This causes high blood sugar levels.
Type 2 diabetes is frequently linked to lifestyle choices such as poor food, lack of exercise, and obesity. While it can appear at any age, it is most typically diagnosed in middle-aged and elderly people. In certain circumstances, Type 2 diabetes can be treated with lifestyle changes such as eating a healthier diet, increasing physical exercise, and decreasing weight. Medicines and insulin therapy may also be recommended to help regulate blood sugar levels.

Causes and Risk Factors of Diabetes
The specific origins of diabetes are unknown, however a number of variables contribute to its development. Type 1 diabetes is thought to be caused by a genetic predisposition as well as environmental factors. In contrast, Type 2 diabetes is frequently linked to lifestyle choices and genetics.
Causes and Risk Factors of Type 1 Diabetes
Type 1 diabetes is assumed to be caused by a mix of genetic predisposition and environmental factors, such as viral infections. People who have a family history of Type 1 diabetes are more likely to get the condition. Several viruses, including enteroviruses and rotaviruses, have been associated to the development of Type 1 diabetes.
Causes and Risk Factors of Type 2 Diabetes
Lifestyle variables such as poor eating, sedentary activity, and obesity all have a significant impact on type 2 diabetes. Excess body weight, particularly around the waist, raises the risk of insulin resistance and Type 2 diabetes. Furthermore, people with a family history of Type 2 diabetes are more likely to develop the disease themselves.
Other risk factors for Type 2 diabetes include age (over 45), a history of gestational diabetes, high blood pressure, and ethnicity (African, Hispanic, Asian, or Pacific Islander).

Symptoms and Diagnosis of Diabetes
The symptoms of diabetes can vary depending on the type and severity of the condition. However, some common symptoms include:
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Fatigue and weakness
- Blurred vision
- Slow-healing wounds
- Tingling or numbness in the hands or feet
If you experience any of these symptoms, it is essential to consult a healthcare professional for a proper diagnosis. They will typically perform a series of tests, including blood sugar level measurements, to determine if you have diabetes and what type it may be.
Impact of Diabetes on Overall Health
Diabetes can have a significant impact on overall health, affecting various organ systems in the body. When blood sugar levels are consistently high, it can lead to several complications, including:
- Cardiovascular disease: Diabetes raises the risk of cardiovascular disease, heart attacks, and strokes.
- Kidney damage: High blood sugar levels can damage the kidneys’ filtering mechanisms, resulting in diabetic nephropathy and, in severe cases, renal failure.
- Nerve damage: High blood sugar levels can eventually damage nerves throughout the body, culminating in diabetic neuropathy. This can lead to discomfort, numbness, and tingling in the extremities.
- Eye problems: Diabetes can damage blood vessels in the eyes, causing diabetic retinopathy, cataracts, and glaucoma. If left untreated, these disorders might result in vision loss or blindness.
- Foot problems: Diabetes can reduce blood flow to the feet, increasing the risk of ulcers, infections, and, in extreme cases, amputation.
Managing diabetes requires a comprehensive approach to minimize the risk of complications. Regular medical check-ups, blood sugar monitoring, medication or insulin therapy, and a healthy lifestyle are crucial components of diabetes management.

Managing Diabetes as a Chronic Health Condition
To effectively manage diabetes, one must take a proactive approach. Successful management requires a combination of medical intervention, lifestyle changes, and continual self-care. Here are some important components of controlling diabetes:
Blood Sugar Monitoring
People with diabetes must monitor their blood sugar levels on a regular basis. This can be accomplished with a blood glucose meter, continuous glucose monitoring (CGM) system, or other tools. Individuals who watch their blood sugar levels can make more educated decisions regarding their food, physical activity, and medication or insulin dosages.
Medications and Insulin Therapy
Depending on the type and severity of diabetes, medicines and insulin therapy may be recommended to help control blood sugar levels. These treatments seek to modulate insulin production, improve insulin sensitivity, or decrease glucose synthesis in the liver. To ensure optimal management, adhere to the indicated treatment plan and consult with a healthcare expert on a frequent basis.
Healthy Eating
Managing diabetes requires a well-balanced diet. This usually entails eating a range of nutrient-dense meals such fruits, vegetables, whole grains, lean meats, and healthy fats. Individuals with diabetes may benefit from portion control and carbohydrate counting, as carbs have a direct effect on blood sugar levels. Working with a licensed dietitian can provide individualized advice on meal planning and nutritional needs.
Regular Physical Activity
Diabetes management relies heavily on physical activity. Regular exercise lowers blood sugar, improves insulin sensitivity, manages weight, and lowers the risk of cardiovascular problems. To get the most out of your workouts, combine aerobic, strength, and flexibility activities. However, it is critical to speak with a healthcare practitioner before beginning any new workout plan, especially if you have any underlying medical concerns.
Stress Management and Emotional Well-being
Managing diabetes can be emotionally difficult, and stress can have a substantial impact on blood sugar levels. Finding healthy ways to cope with stress, such as practicing relaxation techniques, taking up hobbies, or seeking support from friends and family, is critical for general well-being. Furthermore, joining diabetes support groups or seeking professional counseling can provide important emotional support and direction.

Treatment Options for Diabetes
The treatment options for diabetes differ according to the kind and severity of the ailment. While there is currently no cure for diabetes, numerous treatment options aim to effectively manage blood sugar levels while reducing the risk of complications. These therapy options include the following:
Medications
Individuals with Type 2 diabetes are often administered oral medicines to help regulate blood sugar levels. These drugs act by improving insulin sensitivity, boosting insulin production, or decreasing glucose synthesis in the liver. In some circumstances, injectable medicines, such as GLP-1 receptor agonists or SGLT2 inhibitors, may be used to control blood sugar levels.
Insulin Therapy
Individuals with Type 1 diabetes, as well as some cases of Type 2 diabetes, require insulin therapy to adequately regulate blood sugar. Insulin can be delivered via injections or an insulin pump. The dosage and timing of insulin administration are regulated by blood sugar levels, food, physical activity, and other variables. Regular monitoring and adjustment of insulin doses are essential for maintaining stable blood sugar levels.
Lifestyle Modifications
Adopting a healthy lifestyle is an important part of diabetes control. This involves eating a well-balanced diet, exercising regularly, staying at a healthy weight, and dealing with stress. Lifestyle changes can assist to enhance insulin sensitivity, control blood sugar levels, and lower the risk of problems.
Blood Sugar Monitoring
Individuals with diabetes should monitor their blood sugar levels on a regular basis in order to make informed decisions about their treatment and lifestyle. This can be accomplished with a blood glucose meter, continuous glucose monitoring (CGM) system, or other tools. Monitoring enables individuals to spot patterns and make required adjustments to their treatment plan while under the supervision of a healthcare expert.
Conclusion
Understanding the different types of diabetes, the causes and risk factors, and the impact on overall health is crucial for my effective management of this chronic health condition.
By adopting healthy habits, such as regular exercise, maintaining a balanced diet, following prescribed medication or insulin therapy, and attending regular medical check-ups, I can maintain stable blood sugar levels and reduce the risk of complications. Additionally, emotional support, stress management, and maintaining a positive mindset are essential for my overall well-being.
While diabetes may present challenges, it should not define my life. With the right knowledge, support, and self-care, I can live well and thrive despite the challenges of this chronic health condition, diabetes.
Trusted Health, Wellness, and Medical advice for your well-being