Health
What are the Risk Factors for Blocked Arteries in your Neck?
Blocked arteries in the neck, also known as carotid artery disease, can pose serious health risks, including stroke and other cardiovascular complications.
Understanding the risk factors associated with this condition is crucial for early detection, prevention, and effective management. In this article, we will delve into the various risk factors that contribute to blocked arteries in the neck. By recognizing these factors, individuals can take proactive steps to reduce their risk and safeguard their cardiovascular health.
From lifestyle choices to underlying medical conditions, identifying the risk factors provides valuable insight into maintaining optimal vascular health and preventing potential complications associated with carotid artery disease.

Understanding blocked arteries in the neck
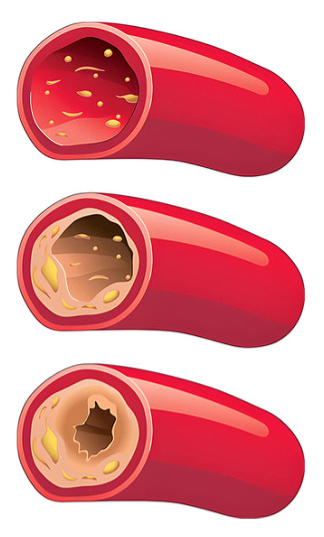
Blocked arteries in the neck, commonly known as carotid artery disease, arise when plaque formation narrows or blocks the carotid arteries that feed blood to the brain. This disorder can reduce blood supply to the brain, increasing the likelihood of a stroke or transient ischemic attack (TIA), often known as a mini-stroke. Understanding the causes, symptoms, and potential implications of blocked arteries in the neck is critical for timely discovery and treatment.
In this post, we will look at the fundamental causes of carotid artery disease, as well as the risk factors, diagnostic procedures, and treatments available. Individuals who understand this illness should take proactive efforts to safeguard their vascular health and lower the risk of stroke-related consequences.
High cholesterol and its role in blocked arteries
High cholesterol contributes significantly to the development of clogged arteries, especially those in the neck. Excess cholesterol in the bloodstream might contribute to plaque formation along the artery walls. Over time, plaque development can restrict the arteries, limiting blood flow to crucial organs including the brain.
High cholesterol levels, when combined with blocked arteries in the neck, might hasten the onset of atherosclerosis, the underlying condition characterized by plaque buildup in the arteries. As plaque deposits accumulate, they might eventually lead to stenosis, or constriction of the carotid arteries.
Furthermore, elevated cholesterol is a major risk factor for cardiovascular illnesses, particularly carotid artery disease. It causes inflammation and oxidative stress in the artery walls, aggravating plaque formation and raising the risk of arterial blockages.
Managing high cholesterol levels through lifestyle changes such as a nutritious diet, regular exercise, and medication as needed is critical for avoiding and treating blocked neck arteries. Furthermore, routine cholesterol monitoring and early treatments can help reduce the risk of problems related to carotid artery disease.
The impact of diabetes on neck artery health
Diabetes has a substantial impact on neck artery health, notably the development of blocked arteries. People with diabetes are more likely to develop atherosclerosis, a disorder marked by the accumulation of plaque in the arteries. This plaque deposition can occur in the carotid arteries of the neck, resulting in carotid artery disease.
Several factors contribute to the increased risk of carotid artery disease in people with diabetes. For starters, diabetes is connected with elevated blood sugar levels, which can cause inflammation and damage to the artery walls, hastening plaque formation. Second, diabetes is frequently associated with additional risk factors for arterial disease, such as high cholesterol, high blood pressure, and obesity, which exacerbates the course of atherosclerosis.
Furthermore, people with diabetes may have complications such as peripheral artery disease, which reduces blood flow to the limbs but can also affect the arteries in the neck. Furthermore, diabetes raises the chance of developing cardiovascular disorders, such as stroke, which can be caused by plaque rupture in the carotid arteries, resulting in blockages or emboli.
Effective diabetes management, including blood sugar control, lifestyle changes, and medication, is critical for maintaining neck artery health and lowering the risk of carotid artery disease consequences. Regular monitoring of blood sugar, blood pressure, and cholesterol levels, as well as routine medical check-ups, can help reduce the impact of diabetes on neck arteries.

Obesity and its contribution to artery blockage
Obesity significantly contributes to artery blockage, including in the neck arteries. Excess body weight, especially visceral fat stored around organs, can lead to metabolic changes that increase the risk of atherosclerosis—the primary cause of artery blockage. Here’s how obesity contributes to artery blockage:
- Increased Inflammation: Adipose tissue secretes inflammatory chemicals, which cause persistent low-grade inflammation throughout the body. This inflammation affects the inner lining of the arteries, making them more prone to plaque development.
- Dyslipidemia: Obesity is frequently associated with high LDL cholesterol and triglycerides, as well as decreased HDL cholesterol. This dyslipidemia promotes the formation of cholesterol-rich plaques within the artery walls, which narrows the arteries over time.
- Insulin Resistance: Obesity is strongly associated with insulin resistance, a condition in which cells become less receptive to insulin’s actions. Insulin resistance encourages the release of more insulin and contributes to metabolic dysfunction, creating a pro-inflammatory and pro-atherogenic milieu.
- Hypertension: Obesity is a major risk factor for hypertension. Excess body weight can increase the burden on the heart and blood vessels, causing the arteries to stiffen and become more prone to plaque formation.
- Increased Risk of Diabetes: Obesity is a significant risk factor for type 2 diabetes. Diabetes increases atherosclerosis through mechanisms such as hyperglycemia, oxidative stress, and inflammation, which worsens arterial blockage.
- Obstructive Sleep Apnea (OSA): Obesity is a major cause of OSA, which is characterized by frequent pauses in breathing while sleeping. OSA has been associated to endothelial dysfunction and increased arterial stiffness, which contribute to atherosclerosis progression.
Addressing obesity through lifestyle modifications, including a balanced diet, regular physical activity, weight loss, and management of comorbid conditions like diabetes and hypertension, is crucial for reducing the risk of artery blockage and its associated complications. Additionally, close monitoring of cardiovascular risk factors and prompt medical intervention are essential for individuals with obesity to mitigate the progression of atherosclerosis and maintain arterial health
The dangers of physical inactivity and its effect on neck arteries
Physical inactivity poses significant dangers to neck arteries and overall cardiovascular health. Here’s how it affects neck arteries:
- Reduced Blood Flow: Physical inactivity causes decreased blood flow throughout the body, including the neck arteries. Regular physical activity improves effective blood circulation, which contributes to the health and flexibility of artery walls. Inactive lifestyles promote slow blood flow, increasing the risk of plaque accumulation and arterial blockage in the neck arteries.
- Promotes Atherosclerosis: Lack of physical activity is a major risk factor for atherosclerosis, which is the accumulation of plaque inside the arteries. Sedentary behavior, such as prolonged sitting or minimal activity, can cause the buildup of fatty deposits in the artery walls, narrowing the arteries and decreasing blood flow. This process is especially harmful to the carotid arteries in the neck, which deliver oxygen-rich blood to the brain.
- Contributes to Risk Factors: Physical inactivity is frequently associated with other risk factors for arterial blockage, including obesity, hypertension, high cholesterol, and diabetes. These factors can cause atherosclerosis both individually and synergistically, increasing the likelihood of plaque formation in the neck arteries.
- Endothelial Function Impairs: Regular physical activity promotes the health and function of the endothelium, which is the inner lining of blood vessels. In contrast, chronic inactivity can compromise endothelial function, resulting in inflammation, oxidative stress, and dysfunction. This malfunction makes the neck arteries more susceptible to plaque formation and raises the risk of cardiovascular events such as stroke and heart attack.
- Physical inactivity promotes metabolic dysfunction: such as insulin resistance and dyslipidemia, which exacerbates atherosclerosis. These metabolic anomalies disturb the equilibrium of lipids and glucose in the bloodstream, creating conditions permissive to plaque buildup and arterial damage.
- Increases the Risk of Thrombosis: Inactive lifestyles are connected with changes in blood clotting processes, which raises the risk of thrombosis—the formation of blood clots within arteries. Thrombotic events can block the neck arteries and impair blood supply to the brain, resulting in an ischemic stroke or a transient ischemic attack (TIA).
Overall, physical inactivity poses grave dangers to neck arteries and vascular health. Adopting a physically active lifestyle, incorporating regular exercise, and reducing sedentary behavior are essential strategies for preserving the health and integrity of the neck arteries, minimizing the risk of atherosclerosis, and safeguarding against cardiovascular disease.
Smoking and its correlation to blocked neck arteries
Smoking has a profound correlation with the development and progression of blocked neck arteries, medically termed carotid artery disease. Here’s how smoking impacts neck arteries:
- Promotes Atherosclerosis: Smoking is a major risk factor for atherosclerosis, a condition marked by the accumulation of fatty deposits (plaques) within arteries. Cigarette smoke contains chemicals that harm the inner lining of the arteries (endothelium) and cause inflammation, making plaque more likely to develop. Atherosclerosis can cause narrowing and occlusion of the carotid arteries, which carry blood to the brain and increase the risk of stroke.
- Increases Plaque Vulnerability: Smoking not only stimulates plaque production but also makes plaques more prone to rupture. When plaques break, blood clots (thrombosis) can form and clog the carotid arteries, resulting in a stroke or transient ischemic attack (TIA), often known as a mini-stroke.
- Elevates Blood Pressure: Smoking causes high blood pressure and heart rate by constricting blood vessels and promoting the production of stress hormones such as adrenaline. Elevated blood pressure puts additional strain on the artery walls, causing endothelial dysfunction and raising the risk of plaque formation and arterial obstruction in the neck.
- Alters Lipid Profile: Smoking alters lipid metabolism, resulting in negative alterations in cholesterol levels. It lowers high-density lipoprotein (HDL) cholesterol, also known as “good” cholesterol, which helps eliminate excess cholesterol from the bloodstream. Smoking also raises low-density lipoprotein (LDL) cholesterol, also known as “bad” cholesterol, which promotes plaque formation in arteries, especially the carotid arteries.
- Reduces Oxygen Delivery: Carbon monoxide, a harmful component of cigarette smoke, attaches to hemoglobin in the bloodstream more easily than oxygen. This lowers red blood cells’ oxygen-carrying capacity, depriving tissues, notably the brain fed by the carotid arteries, of vital oxygen. Reduced oxygen delivery can worsen the effects of carotid artery disease, increasing the likelihood of stroke complications.
- Interferes with Arterial Healing: Smoking has a negative impact on the body’s ability to heal and maintain its blood vessels. It reduces endothelial function, slows wound healing, and inhibits the development of new blood vessels (angiogenesis). As a result, smokers are less likely to benefit from procedures that restore blood flow to the carotid arteries, such as carotid endarterectomy or angioplasty with stenting.
Overall, smoking significantly accelerates the progression of carotid artery disease and heightens the risk of stroke and other cardiovascular complications. Quitting smoking is essential for preserving the health of the neck arteries, reducing the likelihood of arterial blockage, and mitigating the adverse outcomes associated with carotid artery disease.

How age and gender can increase the risk of artery blockage
Age and gender play significant roles in increasing the risk of blocked arteries, including the development of conditions like atherosclerosis and subsequent complications such as heart attacks and strokes. Here’s how age and gender influence this risk:
- Age:
- Cumulative Effect of Risk Factors: As people age, they are more prone to acquire risk factors linked to arterial blockage, such as high blood pressure, high cholesterol, diabetes, and obesity. Over time, these risk factors might contribute to the slow accumulation of plaque within the arteries, limiting their diameter and hindering blood flow.
- Degenerative Changes: Aging is related with blood vessel degeneration, such as arterial wall stiffness and decreased flexibility (arteriosclerosis). These alterations can aggravate hypertension and raise the risk of atherosclerosis, making arteries more susceptible to obstruction.
- Increased Inflammation: Aging is also associated with chronic low-grade inflammation throughout the body, known as inflammaging. Persistent inflammation causes endothelial dysfunction and promotes the production of atherosclerotic plaques, hastening the progression of arterial blockage.
- Decreased Regenerative Capacity: As we age, the body’s ability to repair and regenerate damaged blood vessels declines. Because of their weaker vascular repair systems, older people are more susceptible to the negative consequences of arterial obstruction and less receptive to therapies aimed at restoring blood flow.
- Cumulative Effect of Risk Factors: As people age, they are more prone to acquire risk factors linked to arterial blockage, such as high blood pressure, high cholesterol, diabetes, and obesity. Over time, these risk factors might contribute to the slow accumulation of plaque within the arteries, limiting their diameter and hindering blood flow.
- Gender:
- Hormonal Influence: Estrogen, the principal female sex hormone, protects the cardiovascular system by maintaining healthy blood vessel function and regulating lipid metabolism. Women often have lower rates of arterial blockage before menopause than men of the same age, owing to estrogen’s cardioprotective effects. However, following menopause, when estrogen levels fall, women’s chance of getting arterial blockage approaches that of males.
- Unique Risk Profiles: Males and females may have different risk profiles for arterial blockage. For example, men acquire atherosclerosis at a younger age than premenopausal women, whereas women may suffer a more rapid increase in risk following menopause. Furthermore, women with polycystic ovarian syndrome (PCOS) or a history of pregnancy difficulties such as preeclampsia may be more likely to develop arterial blockage due to underlying metabolic abnormalities and endothelial dysfunction.
- Sociocultural Factors: Sociocultural factors may potentially have an impact on gender discrepancies in artery blockage risk. Men have historically been more prone to engage in behaviors associated with cardiovascular risk, such as smoking and excessive alcohol drinking, which can hasten the development of atherosclerosis. However, when societal standards change and gender-specific risk factors are identified, the cardiovascular risk picture may shift correspondingly.
- Hormonal Influence: Estrogen, the principal female sex hormone, protects the cardiovascular system by maintaining healthy blood vessel function and regulating lipid metabolism. Women often have lower rates of arterial blockage before menopause than men of the same age, owing to estrogen’s cardioprotective effects. However, following menopause, when estrogen levels fall, women’s chance of getting arterial blockage approaches that of males.
Overall, age and gender are important determinants of artery blockage risk, reflecting the complex interplay of biological, hormonal, and sociocultural factors. Understanding these influences can inform risk assessment, preventive strategies, and personalized approaches to managing arterial health across the lifespan.
Family history and its influence on neck artery health
Family history plays a crucial role in determining an individual’s risk of developing blocked arteries in the neck, known as carotid artery disease. Here’s how family history influences neck artery health:
- Genetic Predisposition:
- Individuals with a family history of carotid artery disease are more likely to inherit genetic predispositions that contribute to the development of atherosclerosis, which is the leading cause of arterial blockage. Genetic variables can influence cholesterol metabolism, inflammation, blood clotting processes, and arterial wall shape, all of which contribute to carotid artery plaque formation.
- Certain genetic mutations and variants have been related to an increased risk of atherosclerosis and arterial stenosis (narrowing) in familial cases of carotid artery disease. These genetic characteristics, when combined with environmental influences such nutrition, lifestyle, and exposure to cardiovascular risk factors, can regulate disease progression.
- Individuals with a family history of carotid artery disease are more likely to inherit genetic predispositions that contribute to the development of atherosclerosis, which is the leading cause of arterial blockage. Genetic variables can influence cholesterol metabolism, inflammation, blood clotting processes, and arterial wall shape, all of which contribute to carotid artery plaque formation.
- Shared Lifestyle and Environmental Factors:
- Families frequently share lifestyle patterns and environmental exposures that might affect cardiovascular health. Dietary patterns, physical activity levels, smoking habits, and stress management strategies, for example, are commonly shared by family members living in the same household or community. Unhealthy lifestyle habits, such as a saturated fat-rich diet, sedentary activity, and tobacco use, can all contribute to the development and progression of carotid artery disease.
- Environmental factors such as air pollution, secondhand smoke, and chronic stress in the family setting can all have an impact on artery health and worsen atherosclerosis. Furthermore, socioeconomic circumstances and access to healthcare resources may differ within families, affecting people’s ability to manage cardiovascular risk factors and receive preventative therapies.
- Families frequently share lifestyle patterns and environmental exposures that might affect cardiovascular health. Dietary patterns, physical activity levels, smoking habits, and stress management strategies, for example, are commonly shared by family members living in the same household or community. Unhealthy lifestyle habits, such as a saturated fat-rich diet, sedentary activity, and tobacco use, can all contribute to the development and progression of carotid artery disease.
- Shared Medical Conditions:
- Families may be predisposed to specific medical disorders that raise the incidence of carotid artery disease. These conditions include hypertension, diabetes, hyperlipidemia (high cholesterol), obesity, and metabolic syndrome. Genetic vulnerability, combined with shared environmental impacts, can lead to the clustering of these risk factors within families, raising the total chance of developing artery blockages.
- Inherited connective tissue disorders, such as Marfan syndrome and Ehlers-Danlos syndrome, can predispose people to arterial irregularities and raise their risk of carotid artery dissection, a less common but deadly cause of neck artery obstruction.
- Families may be predisposed to specific medical disorders that raise the incidence of carotid artery disease. These conditions include hypertension, diabetes, hyperlipidemia (high cholesterol), obesity, and metabolic syndrome. Genetic vulnerability, combined with shared environmental impacts, can lead to the clustering of these risk factors within families, raising the total chance of developing artery blockages.
Overall, family history serves as an important risk factor for carotid artery disease, reflecting both genetic predispositions and shared environmental influences within families. Understanding the familial clustering of cardiovascular risk factors can help healthcare providers assess an individual’s overall risk profile, implement preventive measures, and tailor treatment strategies to mitigate the impact of genetic and familial factors on neck artery health.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
Sources Expanded:
Carotid artery disease – Symptoms and causes – Mayo Clinic. (2023, April 19). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/symptoms-causes/syc-20360519
Bruce, D. F. (2008, September 18). Carotid Artery Disease: Causes, Symptoms, Tests, and Treatment. WebMD. https://www.webmd.com/heart-disease/carotid-artery-disease-causes-symptoms-tests-and-treatment
High cholesterol – Symptoms and causes – Mayo Clinic. (2023, January 11). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/symptoms-causes/syc-20350800#:~:text=High%20cholesterol%20can%20cause%20a,Chest%20pain.
Is Obesity a Risk Factor for Carotid Atherosclerotic Disease? (2022). Retrieved March 28, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9144226/
Physical Activity and Characteristics of the Carotid Artery Wall in High‐Risk Patients. (2017). Retrieved March 28, 2024, from https://www.ahajournals.org/doi/10.1161/JAHA.116.005143
Cigarette Smoking Accelerates Carotid Artery. (n.d.). Retrieved March 28, 2024, from https://www.ahajournals.org/doi/full/10.1161/01.str.26.8.1409#:~:text=Because%20of%20the%20similar%20intimal,developing%20carotid%20restenosis%20and%20stroke.
Alsiddig, A. M., & Ali, I. A. (2024, January 25). Effects of Smoking on Intima-Media Thickness of the Common Carotid Artery Using Ultrasonography. Artery Research. https://doi.org/10.1007/s44200-024-00044-w
Goicoechea, S., Walsh, M. J., Soult, M. C., Halandras, P., Bechara, C. F., Aulivola, B., & Crisostomo, P. R. (2022, June 1). Female gender increases risk of stroke and readmission after carotid endarterectomy and carotid artery stenting. Journal of Vascular Surgery. https://doi.org/10.1016/j.jvs.2021.10.034
Association between a family history of diabetes and carotid artery atherosclerosis. (2021). Retrieved March 28, 2024, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8510832/
Tallarita, T. (2023, July 21). Manage your risk of carotid artery disease. Mayo Clinic Health System. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/manage-your-risk-of-carotid-artery-disease
Trusted Health, Wellness, and Medical advice for your well-being



