Health Conditions
Find Out The Common Causes of Urinary Incontinence
Are you tired of worrying about leaks and accidents? Urinary incontinence can be embarrassing and distressing, but you are not alone. In fact, more than 25 million persons in the United States suffer with urine incontinence. Understanding the common causes of urinary incontinence is the first step in determining the best treatment.
Types of Urinary Incontinence
Urinary incontinence can present in a variety of ways, depending on the underlying reason. Understanding the various types of urinary incontinence can aid in determining the underlying causes of your disease and exploring relevant treatment choices.
Stress Urinary Incontinence
Stress urinary incontinence occurs when there is pressure on the bladder, which causes leaking. Physical activity like coughing, sneezing, laughing, and jogging can all contribute to this pressure. The primary cause of stress urinary incontinence is weak pelvic floor muscles.
Pregnancy, childbirth, aging, and fat can all lead to muscular weakness. Furthermore, hormonal changes after menopause might impair bladder control, increasing the likelihood of stress urine incontinence.
Urge Urinary Incontinence
Urge urine incontinence, also known as overactive bladder, is defined as a sudden and urgent urge to urinate, followed by involuntary leaking. This type of incontinence is frequently caused by hyperactive bladder muscles that contract before the bladder is full.
The actual origin of hyperactive bladder muscles is not always known, however some conditions can exacerbate the disease. These include urinary tract infections (UTIs), some drugs, and nerve injury that alters brain-to-bladder impulses. Diabetes, Parkinson’s illness, and multiple sclerosis are all potential causes of urge urine incontinence.

Overflow Urinary Incontinence
Overflow urinary incontinence occurs when the bladder does not fully empty, resulting in frequent or continual dribbling of pee. This type of incontinence is frequently caused by an obstruction or blockage in the urinary tract, such as an enlarged prostate in males or a prolapsed bladder in women.
Certain drugs, nerve injury, and weak bladder muscles can all cause overflow urinary incontinence. In other circumstances, the cause may be due to a medical disease or injury that affects the nerves that regulate bladder function.
Functional Urinary Incontinence
Functional urine incontinence occurs when a person is physically unable to reach the bathroom in time owing to mobility or cognitive limitations, despite the fact that the bladder is working normally. This sort of incontinence is common among those suffering from arthritis, Alzheimer’s disease, or Parkinson’s illness.
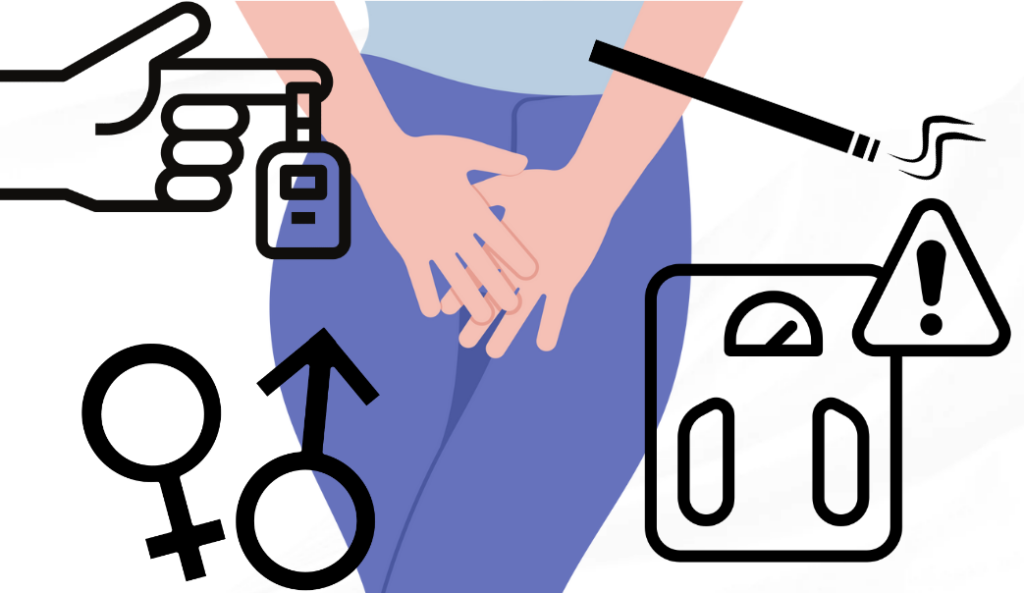
Risk Factors for Developing Urinary Incontinence
While urine incontinence can affect anyone, some variables enhance your chances of having the illness. Understanding these risk factors can help you take preventive steps and seek timely treatment if necessary.
Gender
Pregnancy, delivery, and menopause all increase the likelihood that women will develop urine incontinence. Hormonal changes throughout these stages might weaken pelvic floor muscles and impair bladder control.
Age
As we become older, our muscles, notably the pelvic floor muscles, naturally weaken. This can raise the risk of urine incontinence, particularly in older people.
Obesity
Excess weight can exert strain on the bladder and pelvic floor muscles, causing urine incontinence. Maintaining a healthy weight can help lower your chances of acquiring this illness.
Chronic Health Conditions
Diabetes, Parkinson’s disease, multiple sclerosis, and stroke are all chronic health disorders that can lead to urine incontinence. Managing these disorders successfully can reduce the likelihood of developing incontinence.
Smoking
Smoking has been associated with an increased risk of urinary incontinence. Quitting smoking can improve your general health and lower your risk of having this condition.

Diagnosis and Treatment Options for Urinary Incontinence
If you have urine incontinence, you should visit with a healthcare practitioner to diagnose the underlying causes and discuss treatment options. A complete evaluation, including a medical history, physical examination, and maybe other testing, can assist in determining the particular kind and cause of your urine incontinence.
The treatment options for urinary incontinence depend on the underlying causes and severity of the condition. These may include:
- Lifestyle changes: Making certain adjustments to your lifestyle, such as managing fluid intake, avoiding bladder irritants, and practicing pelvic floor exercises, can help improve bladder control.
- Medications: In some cases, medications may be prescribed to relax the bladder muscles, reduce bladder contractions, or treat underlying infections.
- Medical devices: Certain devices, such as vaginal pessaries or urethral inserts, can help support the bladder and prevent leakage.
- Behavioral therapies: Techniques such as bladder training, biofeedback, and electrical stimulation can help improve bladder control and reduce episodes of incontinence.
- Surgical interventions: In more severe cases or when other treatment options have been ineffective, surgical procedures may be recommended to address the underlying causes of urinary incontinence.
It’s important to remember that treatment plans for urinary incontinence should be personalized to your specific needs and preferences. Working closely with your healthcare provider can help you find the most effective and suitable treatment approach.
Lifestyle Changes and Management Strategies for Urinary Incontinence
In addition to medicinal therapies, there are numerous lifestyle adjustments and management measures that can assist you in better managing urine incontinence and improving your quality of life.
Pelvic Floor Exercises
Regular pelvic floor exercises, or Kegel exercises, can help strengthen the muscles that support the bladder and urethra. These exercises involve squeezing and releasing the pelvic floor muscles, which, when done regularly, can improve bladder control.
Fluid Management
Controlling your fluid intake can assist to minimize the frequency and urgency of urine. It’s crucial to be hydrated, but decreasing fluid intake in the evening can help reduce nighttime toilet excursions.

Bladder Training
Bladder training entails progressively increasing the time between bathroom visits, which helps to stretch the bladder and expand its capacity. This approach can be very beneficial for people who have urge urine incontinence.
Diet Modifications
Certain meals and beverages might irritate the bladder, worsening urine incontinence symptoms. Caffeine, alcohol, spicy meals, and artificial sweeteners are examples of bladder irritants that should be avoided or limited.
Absorbent Products
Using absorbent goods, such as pads or adult diapers, can provide a sense of security while also managing leaks and mishaps. Depending on the severity of your incontinence, you have a variety of alternatives, including inconspicuous pads and more absorbent briefs.
Emotional Support
Living with urine incontinence can be emotionally taxing. Seeking assistance from loved ones, joining support groups, or speaking with a therapist can all provide emotional support and help you manage with the effects of incontinence in everyday life.
Conclusion
Urinary incontinence is a common condition that affects millions of adults worldwide. Understanding the common causes of urinary incontinence, such as weakened pelvic floor muscles, urinary tract infections, overactive bladder muscles, certain medications, and nerve damage, is crucial for finding the appropriate treatment and management strategies.
If I’m experiencing urinary incontinence, I understand that it’s important to consult with a healthcare professional for a proper diagnosis and personalized treatment plan. With the right support and guidance, I can regain control of my bladder and live a more confident and fulfilling life.
Trusted Health, Wellness, and Medical advice for your well-being