Joint Health
How to Diagnose Rheumatoid Arthritis
A disease called rheumatoid arthritis, or RA, causes inflammation in the joints over a long period of time. Most of the time, this inflammation causes pain, stiffness, and swelling. An accurate evaluation must be made as soon as possible in order to provide the best treatment and avoid long-term joint damage.
We will talk about the different methods and tools that doctors use to identify rheumatoid arthritis in this article. Some of these tools and methods are image exams, clinical evaluations, and lab tests. When someone understands the process of diagnosis better, they are more likely to get help early and in the right way, which improves their quality of life even though their sickness is hard to deal with.
Importance of Early Diagnosis
It’s very important to get a diagnosis of rheumatoid arthritis (RA) as soon as possible so that the disease can be managed properly and its long-term effects are kept to a minimum. RA (rheumatoid arthritis) can be treated quickly if it is found early on. This can greatly reduce joint damage, keep functions intact, and improve the general quality of life for people who have the condition.
Furthermore, getting care early on can help stop problems like joint problems and being unable to do things later on. The purpose of this part is to talk about how important early diagnosis is for managing rheumatoid arthritis (RA) and the benefits that early diagnosis offers to both patients and the healthcare system.

Initial Steps in Diagnosing Rheumatoid Arthritis
A full study of the patient’s medical history and a thorough physical exam by a medical professional are the first steps in diagnosing rheumatoid arthritis. Blood tests that measure inflammation markers, like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), are also often done to help with the diagnosis.
The Role of a Physical Exam in Diagnosing Rheumatoid Arthritis
A physical exam is very important for diagnosing rheumatoid arthritis because it checks your general health. Your doctor carefully checks how all of your organs are working, paying special attention to your joints for signs of swelling or stiffness that are common in people with rheumatoid arthritis. In addition, they talk about any specific RA symptoms or worries you have, so they can get a full picture of your health.
The exam also gives the doctor a chance to give the person up-to-date vaccinations and give them personalized advice on how to make changes to their lifestyle or take other actions to improve their general health and joint health, which are both important parts of managing rheumatoid arthritis well.
Appearance of the Patient
- Patients with rheumatoid arthritis usually appear fatigued.
- Vital Signs
- Low-grade fever

Skin
- Rheumatoid nodules can be found on top of bony prominences like the olecranon, the calcaneal tuberosity, the metacarpophalangeal joints, or other places that are constantly under mechanical stress.
- Erythema nodosum – Smooth, red lumps on the shins hurt. Nodules can appear on the legs, arms, trunk, face, neck, or anywhere with fat under the skin. Nodules are 1–5 cm wide and can unite to form enormous hardened areas.
The nodules vary in color from blue-purple to brownish to yellowish to green. This fades like a bruise. The nodules usually heal without pain or scarring in two to six weeks. - Loss of digital skin – A disorder characterized by thin, fragile, and easily injured skin of the fingers and toes. Chronic inflammation and tissue abnormalities from rheumatoid arthritis produce this illness.
The disorder may weaken the skin’s elasticity and protection, leaving it more susceptible to cuts, rips, and ulcers. This can significantly affect the person’s quality of life and daily activities. Preventing digital skin loss and related complications requires proper rheumatoid arthritis treatment, including medication, lifestyle adjustments, and preventative measures. - Palm redness – Palmar erythema may cause this. Rheumatoid arthritis’s inflammation and vascular anomalies increase palm blood flow, causing redness. Warmth and swelling accompany palmar erythema, which might appear as diffuse redness or patches on the palms.
Palmar erythema in rheumatoid arthritis is a non-specific symptom of inflammation, although its cause is uncertain. Managing rheumatoid arthritis with adequate medication is essential for treating palmar erythema. - Thinners that spread out (rice paper skin) – This refers to the skin being thinner and more delicate, similar to rice paper. Chronic inflammation and disease-related connective tissue alterations are common causes of this syndrome.
The skin may appear translucent, making it more susceptible to ripping, bruising, and ulcer formation. This thinning effect can be especially noticeable in areas affected by joint swelling and deformity. Proper rheumatoid arthritis care, including anti-inflammatory and skin-protective drugs, is critical for treating rice paper skin symptoms and avoiding complications. - Beadings on the nails – This refers to little, visible bumps or ridges that can form on the nail bed. These bead-like forms, also known as nail fold infarctions or nail fold capillaroscopy abnormalities, are frequently suggestive of underlying microvascular alterations caused by the disease. In rheumatoid arthritis, inflammation can disrupt the small blood vessels in the nail folds, causing changes in blood flow and the appearance of these beads.
While not unique to rheumatoid arthritis, their presence can be used as an additional clinical indicator of disease activity. Monitoring nail changes, as well as other symptoms, helps to manage and analyze the development of rheumatoid arthritis.
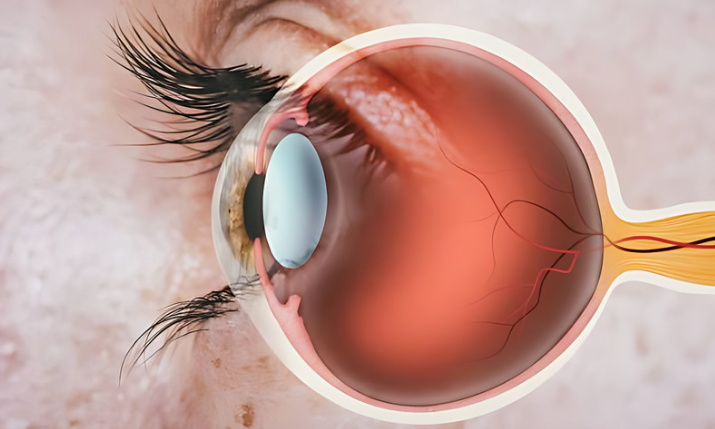
Eyes
- Dry eyes – These eye symptoms are common due to inflammation and immune system dysfunction. Keratoconjunctivitis sicca, or dry eye syndrome, causes eye pain, redness, and irritation due to decreased tear production or increased tear evaporation.
Systemic inflammation in RA can affect lacrimal glands, exacerbating dry eye symptoms. RA treatment, including anti-inflammatory medicines and eye drops to lubricate, is essential for dry eye symptoms and ocular health. Managing dry eye in rheumatoid arthritis requires regular ophthalmological monitoring. - Scleritis – Scleritis causes inflammation of the eye’s white coating. Rheumatoid arthritis’s inflammatory reaction can produce scleritis.
Eye pain, redness, and light sensitivity are scleritis symptoms. Avoiding vision loss requires prompt diagnosis and treatment. To minimize inflammation and discomfort, corticosteroids and immunosuppressants are often utilized. Rheumatologists and ophthalmologists must work together to treat scleritis in RA patients. - Scleromalacia – The eye’s protective sclera shrinks and deteriorates in uncommon cases of rheumatoid arthritis (RA). Thinning or “melting” of the sclera increases the risk of perforation and vision loss.
Scleromalacia in RA may be caused by eye inflammation. Early diagnosis and treatment prevent issues and preserve vision. medication usually involves corticosteroids and immunosuppressants to reduce inflammation and frequent monitoring by an ophthalmologist to adjust medication.

Lungs
On Auscultation of lungs, these are noticeable in patients with rheumatoid arthritis:
- Decreased breath sounds on both sides – This could indicate pleurisy, a disorder in which the lining of the lungs becomes irritated. In rheumatoid arthritis, inflammation can affect the lungs, resulting in pleurisy, which can cause reduced breath sounds because the inflamed lining restricts lung movement.
This symptom should trigger an immediate medical evaluation to assess lung function and establish appropriate treatment, which may include anti-inflammatory drugs to relieve discomfort. Regular monitoring and collaboration between rheumatologists and pulmonologists are critical for controlling pulmonary problems in people with rheumatoid arthritis. - Crackles may be present – This could indicate the presence of interstitial lung disease (ILD), which is a typical consequence of RA. These unusual lung sounds, which sound similar to Velcro being ripped apart, indicate the presence of fluid or inflammation in the tiny airways or lung tissue. If not treated, ILD can cause progressive scarring and reduced lung function.
Prompt examination by a healthcare practitioner is critical for determining the severity of ILD and initiating appropriate treatment, which may include drugs to reduce inflammation and preserve lung function. Regular monitoring and communication between rheumatologists and pulmonologists are required to properly manage pulmonary problems in rheumatoid arthritis.
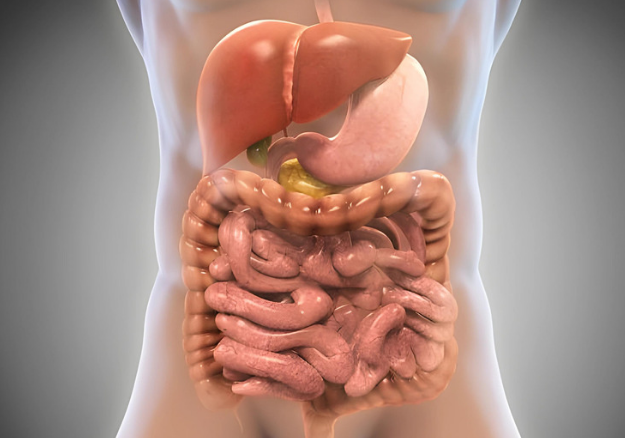
Abdomen
On palpation:
- Hepatomegaly – Rheumatoid arthritis (RA) can cause liver enlargement. In some situations, prolonged RA inflammation can cause liver involvement, resulting in hepatomegaly. This growth could be discovered during a physical checkup by a healthcare expert.
While the exact pathways between RA and hepatomegaly are unknown, frequent monitoring and collaboration between rheumatologists and hepatologists is critical for managing this complication and addressing any underlying liver-related disorders in people with rheumatoid arthritis. - Splenomegaly – Spleen enlargement is occasionally seen in rheumatoid arthritis (RA) due to chronic inflammation and immune system dysfunction. While splenomegaly is uncommon in RA, it can occur due to the disease’s systemic nature, in which inflammation affects multiple organs, including the spleen.
This growth could be discovered during a physical checkup by a healthcare expert. Although splenomegaly in RA is frequently asymptomatic, regular monitoring and collaboration between rheumatologists and healthcare providers are required to manage this consequence and address any underlying disorders associated with spleen enlargement.
Extremities
On inspection
- Redness and swelling of the affected joints – These are common signs of inflammation and immune system malfunction. The inflammation increases blood flow to the joint, causing redness, warmth, and swelling. These symptoms generally appear symmetrically in many joints, including the fingers, wrists, and knees. Redness and swelling can cause discomfort, stiffness, and decreased joint mobility, negatively influencing an individual’s quality of life. Early diagnosis and therapy are critical for managing inflammation and preventing long-term joint damage in rheumatoid arthritis.
On palpation
- Tenderness – Joint redness and swelling indicate inflammation and immune system dysfunction. Inflammation increases joint blood flow, creating redness, warmth, and swelling.
Most joints, including fingers, wrists, and knees, show symmetrical symptoms. Pain, stiffness, and decreased joint mobility can lower a person’s quality of life due to redness and swelling. Managing inflammation and minimizing joint damage in rheumatoid arthritis requires early diagnosis and treatment. - Pain on movement – These are frequent joint inflammation and damage symptoms. RA patients may experience pain when moving their hands, wrists, knees, or feet. Stiffness, edema, and reduced range of motion may accompany mild to severe discomfort.
RA patients’ daily lives and quality of life might be affected by mobility pain. Drugs, physical therapy, and joint protection procedures improve inflammation, discomfort, and joint function in rheumatoid arthritis patients, enhancing well-being. Effective RA pain management and disease control require regular healthcare-provider communication. - Reduced mobility – This limits joint mobility in sick joints. In RA, joint inflammation and damage to the synovial lining can produce stiffness, edema, and discomfort, limiting movement. This reduced motion usually affects minor joints like the hands, wrists, and ankles, but it can also affect major joints like the knees and shoulders.
Reduced range of motion can affect daily life and quality of life over time. RA treatments such as medicines, physical therapy, and lifestyle changes aim to reduce inflammation, relieve symptoms, and restore joint function to restore mobility. Effective management of rheumatoid arthritis symptoms including reduced range of motion requires regular monitoring and contact with healthcare professionals.

Gathering Medical History for Accurate Diagnosis
A complete medical history is necessary to correctly diagnose rheumatoid arthritis because it helps doctors understand when the symptoms started, how long they lasted, how they got worse, and if there is a history of autoimmune illnesses in the patient’s family.
Additionally, learning about a person’s past medical conditions, medication background, and lifestyle choices can help rule out other conditions and make treatment plans that fit their unique needs.
Laboratory Tests for Rheumatoid Arthritis
- Rheumatoid Factor (RF) – This blood test detects RF, an antibody that many people with rheumatoid arthritis may eventually carry in their blood. An antibody is a type of protein produced by the immune system to help combat invaders in the body. Not everyone with RA tests positive for RF; some test positive but never develop the disease, while others test positive but have another condition. Doctors can, however, utilize this test in conjunction with other test results and observations to diagnose rheumatoid arthritis.
- Anti-cyclic citrullinated peptide antibodies (anti-CCP) – This blood test detects anti-CCP antibodies, which are present in many persons with rheumatoid arthritis patients. Furthermore, anti-CCP can surface before RA symptoms occur, allowing doctors to diagnose the condition earlier. This test’s results, together with those from RF blood testing, are extremely effective in validating a rheumatoid arthritis diagnosis. However, it is crucial to note that some patients have rheumatoid arthritis despite normal blood testing.
- Complete Blood Count – This blood test counts different types of blood cells and can help diagnose anemia, which is frequent in persons with RA.
- Erythrocyte sedimentation rate – This test detects inflammation in the body and tracks illness activity and response to treatment.
- C-reactive protein – This is another frequent inflammation test that can be used to diagnose rheumatoid arthritis as well as to evaluate disease activity and treatment response.
- Other blood tests – Your doctor may also perform other tests to assess your kidney function, electrolytes, liver function, thyroid function, muscle markers, other autoimmune markers, and infection markers in order to assess your overall health and make further diagnoses. Other particular diagnostics for rheumatoid arthritis are occasionally suggested.

Imaging Tests for Rheumatoid Arthritis
Imaging tests, together with a physical exam and laboratory tests, can aid in the diagnosis of RA. These imaging tests may help to diagnose RA.
X-ray – This can reveal bone deterioration, a hallmark of RA, where bones connect at joints. They are a common diagnostic technique; however, because inflammation-related damage accumulates over time and may not be seen on an X-ray early on, they may be ineffective for diagnosing early RA.
Magnetic resonance imaging, or MRI – This is a process that uses radio waves and a strong magnet connected to a computer to generate 3D images of internal body components. MRIs can reveal abnormalities in cartilage and bone that are suggestive of RA.
Ultrasound – Often known as sonography, ultrasound, is a technique that employs sound waves to make images of inside body components. This can be utilized to detect changes in bones and cartilage that are indicative of RA before they appear on an X-ray. Other advantages of ultrasonography include its inexpensive cost and the fact that it does not expose the body to radiation, unlike X-rays.
Computed tomography (CT) scan – This is an imaging process that combines a succession of X-ray images to produce cross-sectional images of various body areas. According to studies, CT scans may be useful for detecting early bone degradation associated with RA.

Additional Diagnostic Methods
As part of a more thorough approach to diagnosing rheumatoid arthritis (RA), doctors may use imaging techniques other than the usual ones.
Positron emission tomography (PET) scans, which use nuclear tracers, are a great way to find areas of active inflammation. This lets doctors precisely locate the disease and keep an eye on it in RA patients. Using a radioactive substance during bone scans can help find areas with more bone turnover and inflammation. This makes it easier to get a full picture of how RA is progressing and how it affects spine health.
Dual-energy X-ray absorptiometry (DEXA) scans are usually used to check bone density in conditions like osteoporosis. However, they can also be used to check bone health and fracture risk in people with RA, which helps doctors make more complete treatment plans that are right for each patient. Using these advanced imaging methods in the diagnosis and tracking of rheumatoid arthritis helps us understand the disease’s pathology better and make treatment decisions that are more likely to improve patient outcomes.

Seeking Professional Help for Diagnosis
Rheumatologists, as specialized physicians, have the skills required to effectively diagnose rheumatoid arthritis (RA) and give the best treatment options. They use a variety of diagnostic procedures to confirm RA, including screening for particular antibodies such as rheumatoid factor and anti-citrullinated peptides (anti-CCP), both of which are higher in RA patients. These antibody tests are critical in the diagnostic phase, assisting rheumatologists in establishing the existence of RA and initiating appropriate treatment strategies specific to each patient’s needs.
Medical History
When you have rheumatoid arthritis (RA), it is critical to communicate your whole medical history to your doctor. Your medical history includes critical information about potential risk factors, genetic predispositions, and previous illnesses that can affect the course of RA and treatment decisions. Information about previous treatments, surgeries, allergies, and drugs, including over-the-counter vitamins and herbal therapies, allows your doctor to make more informed decisions about pharmaceutical options and any interactions.
Furthermore, information regarding your family’s history of autoimmune disorders might help you understand your risk of developing RA and other similar conditions. By freely sharing your medical history with your doctor, you enable them to give personalized care targeted to your specific health needs, resulting in more effective rheumatoid arthritis management and general well-being.
Remember to tell your doctor:
- Describe your symptoms, when and how they began, and how they have evolved over time.
- What limitations in activities you may have, such as difficulty with work, leisure, or activities around the house.
- About your other medical problems.
- If any of your family members have identical symptoms or suffer from rheumatoid arthritis.
- What medications you are taking.
Answers to these questions can help your doctor make a diagnosis and understand the impact the disease has on your life.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
Sources Expanded
- Rheumatoid arthritis – Diagnosis and treatment – Mayo Clinic. (2023, January 25). https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653
- Branch, N. S. C. A. O. (2023, July 27). Rheumatoid Arthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/rheumatoid-arthritis/diagnosis-treatment-and-steps-to-take
- Rheumatoid Arthritis | CDC. (n.d.). https://www.cdc.gov/arthritis/types/rheumatoid-arthritis.html
- Facr, S. K. M. R. M. M. F. (n.d.). Rheumatoid Arthritis (RA): Practice Essentials, Background, Pathophysiology. https://emedicine.medscape.com/article/331715-overview
- Professional, C. C. M. (n.d.). Physical Examination. Cleveland Clinic.
https://my.clevelandclinic.org/health/diagnostics/17366-physical-examination - Professional, C. C. M. (n.d.). Rheumatoid Arthritis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
- Branch, N. S. C. A. O. (2023, July 27). Rheumatoid Arthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/rheumatoid-arthritis/diagnosis-treatment-and-steps-to-take
- Testing for Rheumatoid Arthritis | Arthritis Foundation. (n.d.). https://www.arthritis.org/diseases/more-about/testing-for-rheumatoid-arthritis
Trusted Health, Wellness, and Medical advice for your well-being



