Health Conditions
Lupus: Unraveling its Effects on the Body
Lupus is a complicated autoimmune disease characterized by the immune system wrongly targeting healthy tissues and organs, resulting in a wide range of symptoms that can affect almost any region of the body.
This disease has a wide-ranging and frequently unpredictable influence on the joints, skin, kidneys, and cardiovascular system. Understanding how this unrelenting Lupus disease affects the body necessitates a thorough examination of its pathophysiology and the various ways it might present.
In this article, we will look at the physiological mechanisms that underpin lupus, as well as the specific organs and systems that it frequently affects, to throw light on the complex nature of this chronic disorder and its profound implications for those who live with it.

Understanding Lupus as a Chronic Autoimmune Disease
Lupus is a chronic autoimmune disease that produces inflammation and pain throughout the body. It is a complicated condition that can affect several organs and systems, including the skin, joints, kidneys, and neurological system.
Autoimmune Mechanism
In autoimmune diseases such as lupus, the immune system misidentifies healthy cells and tissues as foreign intruders and assaults them. This causes chronic inflammation and tissue damage. In lupus, the immune system creates antibodies that attack numerous sections of the body, including DNA, blood cells, and tissue.
Lupus is thought to be caused by a combination of genetic, environmental, and hormonal factors, however, the specific origin is unknown. Certain triggers, such as infections, stress, and sun exposure, can exacerbate lupus symptoms.
Types of Lupus
Lupus is classified into various types: systemic lupus erythematosus (SLE), cutaneous lupus, drug-induced lupus, and neonatal lupus. SLE is the most frequent and severe type of lupus, affecting several organs and systems in the body.
Cutaneous lupus primarily affects the skin, resulting in rashes and lesions. Certain drugs might cause drug-induced lupus, which often disappears once the prescription is discontinued. Neonatal lupus affects babies and is usually transient, lasting a few months.
In conclusion, lupus is a chronic autoimmune disease that produces inflammation and pain throughout the body. It is a complicated condition that can affect several organs and systems, and the specific etiology is unknown. Lupus has no cure, but early diagnosis and treatment can help manage symptoms and prevent complications.
Effects of Lupus on the Body
Lupus is a chronic autoimmune disease that can affect several organs in the body. The following are some of the common impacts of lupus on the body:
Joint and Muscle Impact
Lupus can lead to joint discomfort, stiffness, and edema. It can also cause arthritis, which is inflammation of the joints. Lupus-related arthritis can affect any joint in the body, but it primarily affects the fingers, hands, wrists, and knees. Lupus can induce muscular discomfort and weakness, as well as joint pain.
Skin Manifestations
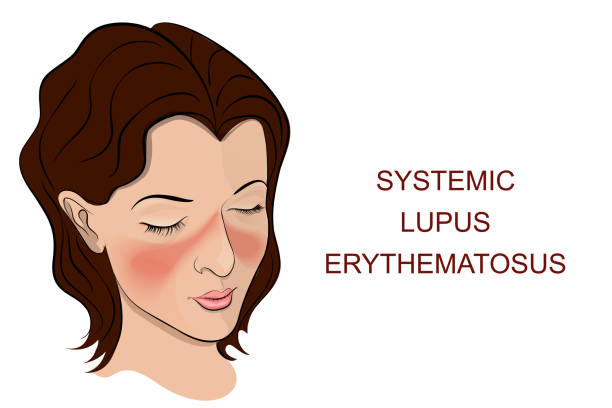
One of the most distinguishing features of lupus is a butterfly-shaped rash on the face that covers the cheekbones and bridge of the nose. Lupus can, however, cause rashes all over the body, as well as hair loss, mouth sores, and sun sensitivity.
Kidney involvement
Lupus can inflame the kidneys, resulting in renal damage and possibly failure. This is one of the most dangerous complications of lupus and must be closely monitored by a doctor.
Cardiovascular Complications
Lupus increases the risk of heart disease, stroke, and blood clots. It can also induce inflammation of the blood vessels, resulting in vasculitis.
Neurological Effects
Lupus can damage the central nervous system, which includes the brain and spinal cord. It can cause migraines, convulsions, and cognitive impairment. Lupus can also harm the peripheral nervous system, which includes the nerves that regulate movement and feeling in the arms and legs. This can produce numbness, tingling, and weakness in the limbs.
Finally, lupus can cause a variety of physical symptoms, including joint pain, skin rashes, renal problems, and neurological issues. Lupus patients must work closely with their doctors to manage their symptoms and avoid complications.
Symptoms and Diagnosis For Lupus
Identifying Symptoms
Lupus is a chronic autoimmune disease that affects the skin, joints, kidneys, and other organs. Its symptoms can vary greatly from person to person and fluctuate over time. Lupus disease’s most common symptoms include joint pain, stiffness, edema, fatigue, fever, headaches, sores, rashes, hair loss, and anemia.
One of the most well-known lupus symptoms is a butterfly rash on the face that covers the cheeks and bridge of the nose. However, not everyone with lupus develops this rash, and some may experience other forms of rashes or skin disorders.
Diagnostic Process
If someone has symptoms that imply they have lupus, they should consult a doctor for an evaluation. In general, lupus is diagnosed using a medical history, physical examination, and laboratory investigations.
During the physical examination, the doctor will search for lupus symptoms such as rashes and joint pain. They may also inquire about the patient’s medical history and family history of autoimmune disorders.
Blood tests are commonly used to diagnose lupus. The antinuclear antibody (ANA) test is a standard blood test that can determine whether a person’s immune system is creating antibodies that attack their own cells and tissues. Other blood tests may be used to detect specific antibodies or to assess organ function.
If a doctor suspects someone has lupus, they may refer them to a rheumatologist, a specialist in autoimmune diseases. A rheumatologist may conduct additional tests and exams to confirm the diagnosis and devise a treatment plan.

Management and Prognosis for Lupus
Treatment Approaches
There is currently no cure for lupus, although medication can help manage symptoms and avoid consequences of this disease. Treatment is usually personalized to the individual and may include a combination of drugs, lifestyle changes, and additional therapies.
Nonsteroidal anti-inflammatory medicines (NSAIDs), corticosteroids, antimalarials, immunosuppressants, and biologics are among the most regularly used medications for lupus. These drugs can help to reduce inflammation, alleviate pain, and suppress the immune system.
In addition to drugs, lifestyle adjustments such as regular exercise, a nutritious diet, and avoiding sun exposure can aid in symptom management and flare prevention. Meditation, yoga, and counseling are all stress management practices that might be beneficial.
Living with Lupus
Living with lupus might be difficult, but it is possible to control the condition and live a full life. Individuals with lupus should collaborate closely with their healthcare physician to design a treatment plan that is appropriate for them.
Individuals with lupus should also take care of themselves by getting adequate sleep, eating a balanced diet, and avoiding triggers like stress and sun exposure. Regular check-ups and symptom monitoring can help spot troubles early on and prevent significant health issues.
Potential Complications
Lupus can affect multiple sections of the body and cause a range of consequences. Lupus’ most prevalent complications include kidney failure, cardiovascular disease, and pulmonary hypertension.
Other lupus consequences include blood clots, antiphospholipid antibodies, and cognitive problems. Lupus patients may be concerned about infections like pneumonia because the disease weakens the immune system.
Overall, the prognosis for people with lupus varies depending on the degree of the disease and the organs affected. However, with correct medication and management, many lupus patients can live healthy and fulfilling lives.
Conclusion
Finally, the intricacies of lupus highlight the significant challenges it poses to individuals and the medical community alike.
This disease requires a comprehensive approach to management and care due to its continuous assault on multiple organs and systems, as well as the unpredictable nature of its symptoms. While great progress has been achieved in understanding and treating this autoimmune disease, much more needs to be understood.
Continued research is critical not only for unlocking the secrets of lupus, but also for discovering more effective treatments and, ultimately, achieving a future in which individuals affected can live with greater comfort and resilience.
We can develop routes to better outcomes and a higher quality of life for those dealing with lupus by continued collaboration among patients, healthcare professionals, and researchers.
Trusted Health, Wellness, and Medical advice for your well-being


