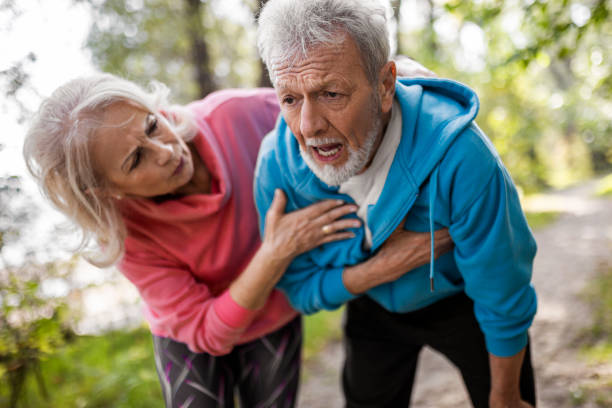
Heart Health
The Link Between Heart Failure and Edema
Heart failure, a condition in which the heart is unable to pump blood adequately, frequently causes the accumulation of fluid in various regions of the body, known as edema. This happens when the weakening heart is unable to circulate blood properly, causing pressure to build up in the blood arteries that lead to the kidney. As a result, the kidneys retain more sodium and water than is required, causing fluid buildup in the body’s tissues, notably in the legs, ankles, and abdomen. Understanding the underlying mechanisms that contribute to edema is critical for properly managing this condition and enhancing the quality of life for people with heart failure.
Understanding Heart Failure
Heart failure is a medical disorder in which the heart is unable to pump blood efficiently. This can cause fluid buildup in numerous regions of the body, such as the lungs, legs, and abdomen. Heart failure can be caused by a variety of reasons, including excessive blood pressure, coronary artery disease, and valve abnormalities.
Pathophysiology of Heart Failure
A healthy heart pumps blood through the arteries and veins, supplying oxygen and nourishment to the body’s tissues. The heart muscle contracts and relaxes in rhythm, moving blood throughout the circulatory system. However, with heart failure, the heart muscle weakens or stiffens, making it difficult for the heart to pump blood efficiently.
Heart failure is classified into two types: systolic and diastolic. Systolic heart failure occurs when the heart muscle weakens and fails to contract efficiently, limiting the volume of blood that can be pushed out of the heart. In diastolic heart failure, the heart muscle stiffens and cannot relax adequately, limiting the amount of blood that can be filled in the heart.
Types of Heart Failure
Heart failure can be characterized according to which side of the heart is affected. Left-sided heart failure occurs when the left side of the heart fails to pump blood adequately, resulting in fluid buildup in the lungs. Right-sided heart failure occurs when the right side of the heart fails to pump blood adequately, resulting in fluid buildup in the legs, abdomen, and other regions of the body.
Overall, heart failure is a complicated medical illness that can significantly impair a person’s quality of life. Understanding the pathophysiology of heart failure and the many forms of heart failure can assist healthcare providers in developing effective treatment approaches to improve patient outcomes.

Mechanisms of Edema in Heart Failure
Edema is a typical symptom of heart failure, produced by fluid accumulation in the body’s tissues. Heart failure can cause edema through a variety of processes, including fluid accumulation and blood pressure fluctuations, venous congestion, and capillary dynamics.
Fluid Buildup and Blood Pressure
The heart’s main duty is to pump blood throughout the body. Heart failure impairs the heart’s ability to pump blood, resulting in a decrease in blood flow. This restriction in blood flow can cause the body to retain fluid, resulting in edema. Furthermore, the restriction in blood flow might cause blood pressure to rise, resulting in additional fluid buildup.
Venous Congestion and Capillary Dynamics
Venous congestion is another mechanism that can cause edema in patients with heart failure. In heart failure, the heart’s capacity to pump blood efficiently might cause blood to pool in the veins, resulting in venous congestion. This congestion can raise pressure within the veins, resulting in fluid buildup in the surrounding tissues.
Capillary dynamics can potentially cause edema in heart failure. Capillaries are the body’s smallest blood arteries, which exchange nutrients and waste materials between the blood and tissues. In heart failure, decreasing blood flow can cause capillaries to leak, allowing fluid to enter the surrounding tissues.
To summarize, heart failure can cause edema through a variety of processes, including fluid accumulation and blood pressure fluctuations, venous congestion, and capillary dynamics. Understanding these mechanisms may aid in the development of effective treatments for edema in heart failure patients.

Symptoms and Diagnosis
Identifying Edema
Edema, a common symptom of heart failure, is caused by fluid accumulation in the body’s tissues. It is characterized by swelling in the legs, ankles, feet, and abdomen. The swelling may be associated with pain or discomfort, and the skin may appear stretched or glossy. Pitting edema is a type of swelling that causes an indentation when squeezed.
Clinical Evaluation of Heart Failure
The clinical evaluation of heart failure includes a detailed review of the patient’s medical history, a physical examination, and diagnostic testing. The evaluation seeks to discover the underlying cause of heart failure and assess the severity of the problem.
Heart failure symptoms may include shortness of breath, weariness, coughing, and swelling in the legs, ankles, or feet. The intensity of these symptoms varies according to the amount of heart failure.
During the physical examination, the healthcare professional may search for signs and symptoms of heart failure, such as an enlarged heart, abnormal heart sounds, or fluid accumulation in the lungs. Diagnostic procedures, such as an electrocardiogram (ECG), echocardiography, and blood tests, may also be used to assess the heart’s function and discover any underlying disorders that may be contributing to heart failure.
Finally, detecting edema and doing a clinical evaluation of heart failure are critical steps in diagnosing and managing heart failure. If you suffer any of the aforementioned symptoms, seek medical attention right once.

Treatment and Management
Medical Interventions
There are various medications available to treat edema caused by heart failure. Initially, diuretics are used to help the body eliminate excess fluid. Diuretics work by increasing urine flow while decreasing fluid retention in the body. Furosemide, torsemide, and bumetanide are some of the most commonly used diuretics for heart failure.
In addition to diuretics, other medications can be used to treat heart failure and its symptoms. ACE inhibitors and ARBs are drugs that reduce blood pressure and improve heart function. Beta-blockers can lower heart rate and reduce strain on the heart. Mineralocorticoid receptor antagonists (MRAs) can help reduce fluid retention while improving heart function.
Lifestyle Adjustments and Supportive Care
Lifestyle adjustments and supportive care, including medication, can help treat edema caused by heart failure. For example, patients may be advised to reduce their salt intake because too much salt might promote fluid retention. Patients may be advised to limit their fluid intake, particularly if they have considerable swelling.
Exercise can also help you manage heart failure and its symptoms. While people with severe heart failure should limit their physical activity, moderate exercise can help improve heart function and reduce fluid retention. Compression stockings can also help to control edema by boosting circulation and decreasing swelling.
Overall, there are several treatments available for edema induced by heart failure. Patients can improve their quality of life and control their symptoms by working with their healthcare provider to create a personalized treatment plan.
Conclusion
Finally, recognizing the relationship between heart failure and edema is critical for both patients and healthcare practitioners. Edema is a typical indication of heart failure, caused by the heart’s inability to pump blood efficiently. Fluid accumulation in the body’s tissues can cause discomfort and consequences if not managed. Edema management needs a multifaceted approach that includes pharmaceutical management, lifestyle changes, and regular monitoring by healthcare specialists. Individuals suffering from heart failure can improve their overall quality of life by treating the underlying causes of edema and applying suitable treatment measures.
Trusted Health, Wellness, and Medical advice for your well-being


