Health
Treatment Of Persistent Pain in Older Adults
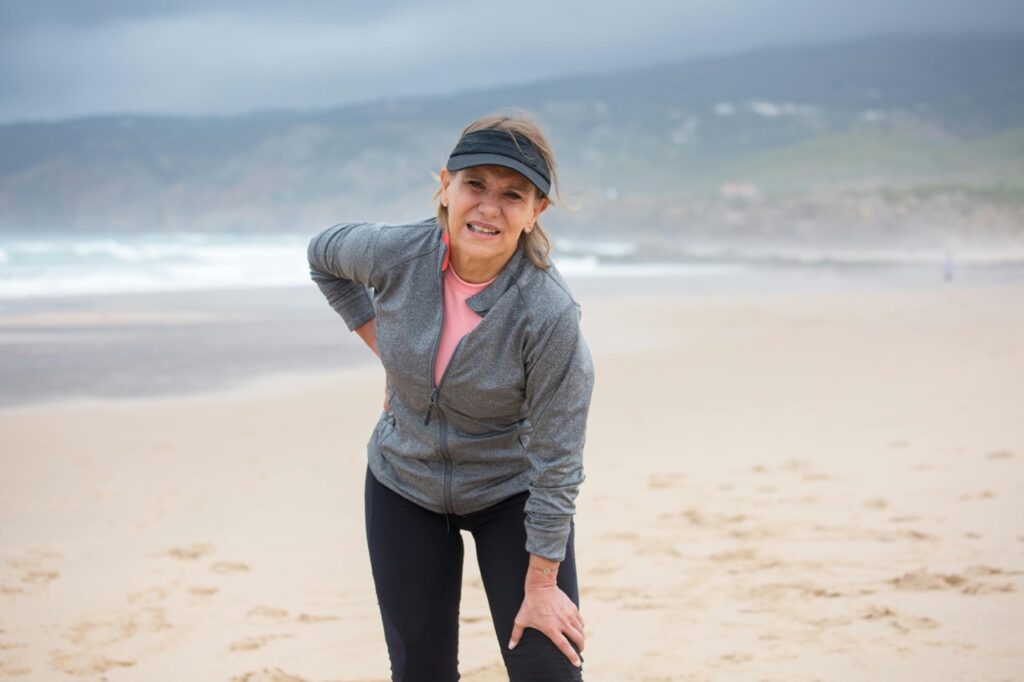
Persistent pain is a typical problem among older persons, and it can have a big influence on their quality of life. According to current research, up to 50% of older persons endure chronic pain, which can cause impaired mobility, sadness, and worry. The prevalence of chronic pain among older adults emphasizes the need for appropriate treatment alternatives to improve their overall health.
The public health implications of chronic pain in older persons cannot be emphasized. Chronic pain can impair all aspects of life, from daily duties to social relationships. It can also result in higher healthcare costs and lower productivity. As a result, it is critical to identify solutions to manage chronic pain in older persons in order to improve their quality of life and minimize the strain on healthcare systems.
Fortunately, there are various therapy options available for chronic pain in older persons. Non-pharmacological therapies, such as exercise and tai chi, have been found to reduce pain severity and frequency. Pharmacotherapy is also a possibility, and it should be tailored to the patient’s specific needs and medical history. As we investigate the different therapy choices available, it is critical to consider the special requirements of older folks and try to improve their overall well-being.

Understanding Persistent Pain in Older Adults
Many older persons suffer from persistent pain, which can be debilitating. Chronic pain becomes more common with age, with up to half of community-dwelling older persons experiencing pain that interferes with their regular function. This section will give an overview of the prevalence and effect of chronic pain in older adults, as well as some of the most frequent painful conditions, risk factors, and comorbidities associated with it.
Prevalence and Impact
Persistent pain is a serious health issue for older persons, significantly reducing their quality of life. Chronic pain can cause sadness, anxiety, social isolation, and financial stress. It can also cause problems with daily tasks including walking, dressing, and bathing, contributing to functional deterioration and loss of independence.
Common Painful Conditions
There are numerous illnesses that might cause chronic pain in older persons. Osteoarthritis is one of the leading causes of persistent pain in older individuals, impacting more than 30 million Americans [4]. Neuropathic pain, caused by nerve injury or malfunction, is another major source of persistent pain in older persons. Cancer, spinal compression fractures, and musculoskeletal diseases are all frequent ailments that can cause chronic pain in older persons.
Risk Factors and Comorbidities
There are various risk factors and comorbidities related with chronic pain in older persons. Comorbidities, such as depression and anxiety, are common in older persons with chronic pain, and they can increase the disease’s impact on quality of life. Social isolation is another risk factor for the development and duration of chronic pain in older persons. Chronic pain can increase healthcare expenses and diminish productivity, therefore the economic burden is a worry.
To summarize, chronic pain is a serious health issue for older persons, with a considerable impact on their quality of life. Osteoarthritis, neuropathic pain, cancer, spinal compression fractures, and musculoskeletal problems are among the most common causes of chronic pain in older persons. Comorbidities, social isolation, and economic stress are among the risk factors related with chronic pain in older persons.

Assessment and Management Strategies
When it comes to managing chronic pain in older persons, there are numerous measures that may be used to reduce suffering and improve quality of life. Here are some important approaches to consider:
Geriatric Pain Assessment
First and foremost, a complete geriatric pain assessment is required to identify the underlying causes of pain and decide the best course of treatment. This may entail reviewing the patient’s medical history, performing a physical exam, and employing a variety of pain assessment techniques to determine the severity and impact of pain. Taking a comprehensive approach to pain evaluation allows us to better personalize our treatment solutions to each patient’s specific needs.
Multimodal Approach to Pain Management
A multimodal approach is another effective option for addressing persistent pain in older persons. This entails adopting a variety of therapies and strategies to address pain from many perspectives. For example, we could combine pharmaceutical and non-pharmacological interventions like exercise, physical therapy, cognitive behavioral therapy, and so on. Using a multimodal strategy allows us to maximize the effectiveness of our pain management solutions while reducing the risk of side effects and complications.
Non-Pharmacological Interventions
Non-pharmacological therapies can be very beneficial in controlling chronic pain in older persons. These may include exercise, physical therapy, occupational therapy, massage treatment, and others. By focusing on non-pharmacological approaches, we can assist patients in managing pain without relying too much on drugs, which can have undesirable side effects and hazards.
Pharmacological Treatments
Of course, pharmaceutical treatments can also play a significant role in controlling persistent pain in older persons. Opioids, acetaminophen, and tramadol are among the most often used pain drugs. However, it is critical to use these medications sparingly and cautiously, taking into account aspects such as dose titration, adverse effects, and the possibility of polypharmacy. Working together with patients and their healthcare professionals allows us to create a pharmaceutical regimen that is safe, effective, and personalized to each patient’s specific needs.
In summary, managing persistent pain in older individuals necessitates a comprehensive, multimodal strategy that considers each patient’s specific requirements and circumstances. By combining various therapies and interventions, we can help patients manage pain more effectively and enhance their overall quality of life.

Challenges in Treatment
When managing persistent pain in older persons, healthcare workers encounter a number of problems. These issues are roughly classified into three categories: polypharmacy and drug interactions, functional impairment and disability, and psychological factors.
Polypharmacy and Drug Interactions
Multiple comorbidities are common in older persons, making it difficult to choose the best medicine, dosage, and treatment regimen. Polypharmacy, or the use of numerous drugs, is frequent among older persons and can raise the risk of severe drug responses and interactions. When treating persistent pain in older persons, it is critical to carefully weigh the risks and benefits of each medicine, as well as keep an eye out for any drug interactions.
Functional Impairment and Disability
Persistent pain in elderly persons can cause functional limitations and disability. Pain can impair mobility, resulting in avoidance of exercise, falls, and solitude. This has the potential to significantly improve the quality of life for elderly persons. When treating persistent pain in older persons, it is critical to evaluate and manage functional impairment and disability.
Psychosocial Factors
Psychosocial factors, such as attitudes and beliefs about pain, can also influence the treatment of chronic pain in older persons. Older persons may have different attitudes and views regarding pain than younger adults, influencing their willingness to follow treatment suggestions. Family members and paid caregivers may also help with the treatment of persistent pain in older adults. These considerations must be considered while designing a treatment plan, and healthcare specialists experienced in psychological therapies should be consulted as needed.
In conclusion, treating persistent pain in older persons can be difficult due to the complicated nature of the problem and their particular demands. When designing a treatment plan, we must carefully weigh the risks and advantages of each choice, assess and manage functional impairment and disability, and consider psychosocial aspects.

Evidence-Based Practice and Education
Evidence-based practice and education are crucial to addressing chronic pain in older persons. We believe that both healthcare professionals and patients benefit from staying current on the newest research, guidelines, and educational programs. In this section, we will look at some of the most significant features of evidence-based treatment and teaching in the context of chronic pain management.
Clinical Guidelines and Systematic Reviews
Systematic reviews and meta-analyses provide a thorough summary of the current state of research on chronic pain management in older persons. They assist us in identifying the most successful treatments and tactics, as well as potential side effects. Healthcare providers can utilize this data to make informed treatment decisions and create personalised care plans for their patients.
Evidence-based guidelines are also important for managing persistent pain. These guidelines were produced through a rigorous process that included a thorough examination of the available information. They give a framework for healthcare practitioners to use when making treatment decisions, ensuring that care is consistent and grounded in the best available evidence.
Educational Initiatives for Healthcare Professionals
Healthcare professionals play an important role in the management of chronic pain in older persons. To guarantee that they have the information and skills needed to deliver excellent care, educational programs are required. These initiatives might take several forms, such as continuing education classes, seminars, and workshops.
Participating in these training efforts allows healthcare practitioners to stay current on the latest research and guidelines, as well as develop new skills and approaches for managing chronic pain. This can eventually lead to better outcomes for patients and a higher quality of life.
Patient and Caregiver Education
Education is not only crucial for healthcare professionals; patients and caregivers must also be taught about chronic pain treatment. Patients and caregivers who understand the nature of chronic pain and the various treatment choices available are better able to make informed decisions about their care.
Patient and caregiver education can take a variety of forms, such as instructional booklets, support groups, and individual therapy. By giving accurate information on persistent pain treatment, we can assist patients and caregivers in making informed decisions about their care, resulting in better results and quality of life.
In conclusion, evidence-based management and education are critical components of addressing chronic pain in older persons. Healthcare professionals and patients can make more educated treatment decisions by remaining up to date on the latest research, recommendations, and educational programs, resulting in better results and quality of life.
Conclusion
In contemplating non-pharmacological interventions, the holistic nature of pain management takes center stage. Integrative modalities, including acupuncture, massage, and cognitive-behavioral therapy, present themselves as viable options. Recognizing the diverse needs of older individuals, these complementary approaches offer avenues for addressing pain beyond the traditional pharmaceutical realm, embracing the importance of mental and emotional well-being in the overall pain management strategy.
Yet, amidst these considerations, the pervasive challenge of stigma surrounding chronic pain in older adults looms large. The misconception that persistent pain is an inevitable part of aging persists, potentially impeding effective communication and intervention. Overcoming this stigma requires a concerted effort to educate healthcare providers, seniors, and their families about the dynamic and treatable nature of persistent pain.
In conclusion, the treatment landscape for persistent pain in older adults demands a nuanced and comprehensive approach. Balancing the benefits and risks of pharmacological interventions, prioritizing physical therapy, incorporating non-pharmacological modalities, and challenging the stigma associated with chronic pain collectively contribute to a more holistic and individualized paradigm of care. As we strive to enhance the well-being of older adults grappling with persistent pain, a collaborative and compassionate approach emerges as paramount, recognizing that each individual’s journey is unique and deserving of tailored, empathetic care.