Medically Accredited
What is Diabetes: Its Types, Causes, Symptoms, and Treatment
Diabetes is a metabolic condition that affects millions of people worldwide, with approximately 38.4 million people in the United States living with it, as presented by the CDC’s (Centers for Disease Control) National Diabetes Statistics Report. It is characterized by high blood sugar levels, either due to inadequate insulin production or impaired insulin function. Read on to learn “what is diabetes“, its causes, types, treatments, and how you can prevent it.
What is Diabetes?
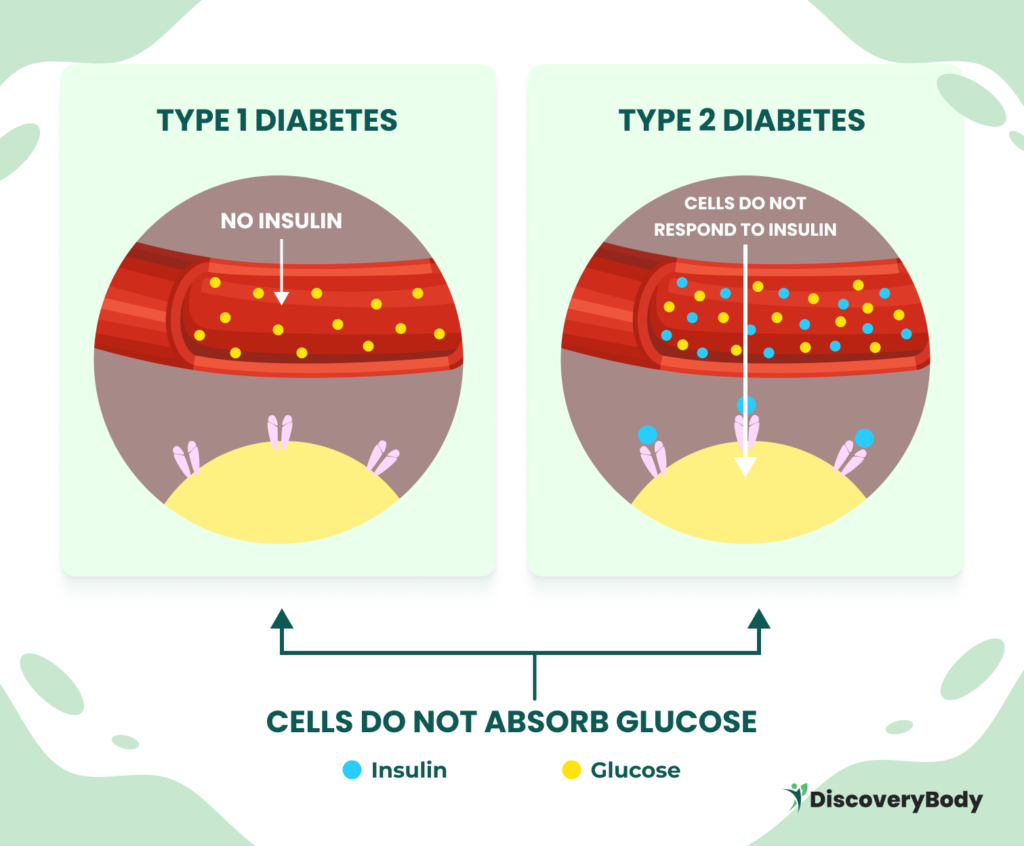
Diabetes, technically termed diabetes mellitus, is a condition that impacts how the body converts food into energy. Most food is broken down into sugar (glucose) and released into the bloodstream, which prompts the pancreas to release insulin. Insulin then directs the muscle, fat, and liver cells to take in the glucose from the bloodstream to convert it to energy or fat for long-term storage.
If the pancreas isn’t making enough insulin or the body isn’t using it properly, glucose builds up in the bloodstream and eventually causes abnormally high blood sugar levels (hyperglycemia). This is how diabetes develops.
It’s important to note that diabetes can affect individuals irrespective of their age. Most forms of diabetes are chronic (long-lasting) but are manageable through medications or lifestyle changes.
What are the types of Diabetes and their Causes?
There are several types of diabetes, each with its own unique characteristics and causes. The most common types include:
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease in which the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. The exact cause of this attack is still unknown. People with type 1 diabetes require insulin injections or the use of an insulin pump to manage their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes is the most prevalent form of diabetes, accounting for about 90% to 95% of all cases. It occurs when the body becomes resistant to insulin or does not produce enough insulin to regulate blood sugar levels effectively. Lifestyle factors, such as a poor diet and a lack of physical activity, play a significant role in the development of type 2 diabetes.
Gestational Diabetes
Gestational diabetes occurs during pregnancy and is characterized by high blood sugar levels that develop due to hormonal changes. It usually resolves after childbirth but increases the risk of developing type 2 diabetes later in life. Managing blood sugar levels during pregnancy is crucial to preventing complications for both the mother and the baby.
Type 1.5 Diabetes
Type 1.5 diabetes, also known as latent autoimmune diabetes in adults (LADA), is a form of diabetes that shares characteristics of both type 1 and type 2 diabetes. It typically develops in adulthood and progresses gradually, resembling type 2 diabetes. However, LADA is an autoimmune condition that can’t be managed solely through lifestyle changes and often requires insulin treatment.
Other Less Common Types of Diabetes
In addition to the main types mentioned above, there are other rare forms of diabetes. Some of these types have specific genetic causes and often require specialized management strategies. Other types of diabetes include:
- Type 3c diabetes: This form of diabetes arises due to damage to the pancreas, which affects its ability to produce insulin. Conditions such as pancreatitis, pancreatic cancer, cystic fibrosis, and hemochromatosis can lead to Type 3c diabetes.
- Maturity-onset diabetes of the young (MODY): MODY is caused by inherited genetic mutations that affect insulin production and usage. This type of diabetes commonly runs in families and affects up to 5% of individuals with diabetes.
- Neonatal diabetes: Neonatal diabetes is a rare form of diabetes that occurs within the first six months of life. It can be a lifelong condition or transient, disappearing after a few months.
- Brittle diabetes: Brittle diabetes is a severe form of Type 1 diabetes characterized by frequent and severe episodes of high and low blood sugar levels.
What are the Symptoms of Diabetes?
The symptoms of diabetes can vary depending on the type and severity of the condition, with symptoms generally more intense in Type 1 diabetes than Type 2 diabetes. However, some common symptoms include:
- Increased thirst and urination
- Unexplained weight loss
- Fatigue and weakness
- Blurred vision
- Slow-healing wounds
- Frequent infections such as urinary tract infections and yeast infections
- Tingling or numbness in the hands or feet
- Dry, itchy skin
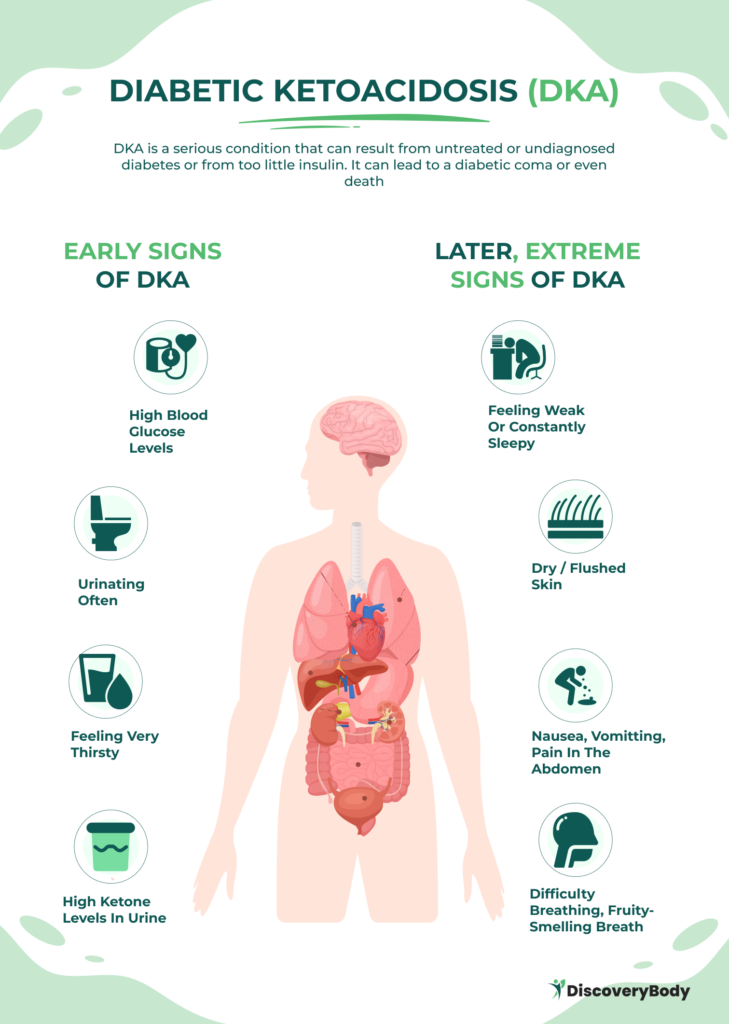
It’s important to note that some people with Type 1 diabetes may also experience symptoms of a severe complication called diabetes-related ketoacidosis (DKA), such as vomiting, stomach pains, fruity-smelling breath, and labored breathing.
In contrast, people with Type 2 diabetes and prediabetes may not have noticeable symptoms or may only have darkened skin on certain body parts (acanthosis nigricans) as a sign.
Still, it’s better to consult with your healthcare provider, as regular check-ups and blood sugar screenings are important for the early detection and management of diabetes.
What are the Risk Factors for Diabetes?
Several risk factors can increase a person’s likelihood of developing diabetes. These include:
Risk factors for Type 1 Diabetes
- Family history: Having a parent or sibling with type 1 diabetes increases the risk.
- Age: Type 1 diabetes is more commonly diagnosed in children and young adults.
Risk factors for Type 2 Diabetes
- Overweight or obesity: Excess body weight is a significant risk factor for type 2 diabetes.
- Sedentary lifestyle: Lack of physical activity and prolonged sitting increase the risk.
- Family history: Having a close family member with type 2 diabetes increases the risk.
- Age: The risk of type 2 diabetes increases with age, especially after the age of 45.
- Gestational diabetes: Women who have had gestational diabetes in previous pregnancies are at a higher risk.
- Prediabetes: Having prediabetes, a condition in which blood sugar levels are higher than normal but not yet in the diabetes range, increases the risk of developing type 2 diabetes.
Risk factors for Gestational Diabetes
- Overweight or obesity: Being overweight before pregnancy increases the risk.
- Age: The risk of gestational diabetes increases with age.
- Previous gestational diabetes: Women who have had gestational diabetes in previous pregnancies are more likely to develop it again.
- Family history: Having a close family member with type 2 diabetes increases the risk.
- Polycystic ovary syndrome (PCOS): Women with PCOS have an increased risk of gestational diabetes.
- Race: Compared to women of other races and ethnicities, Asian women are more likely to develop gestational diabetes.
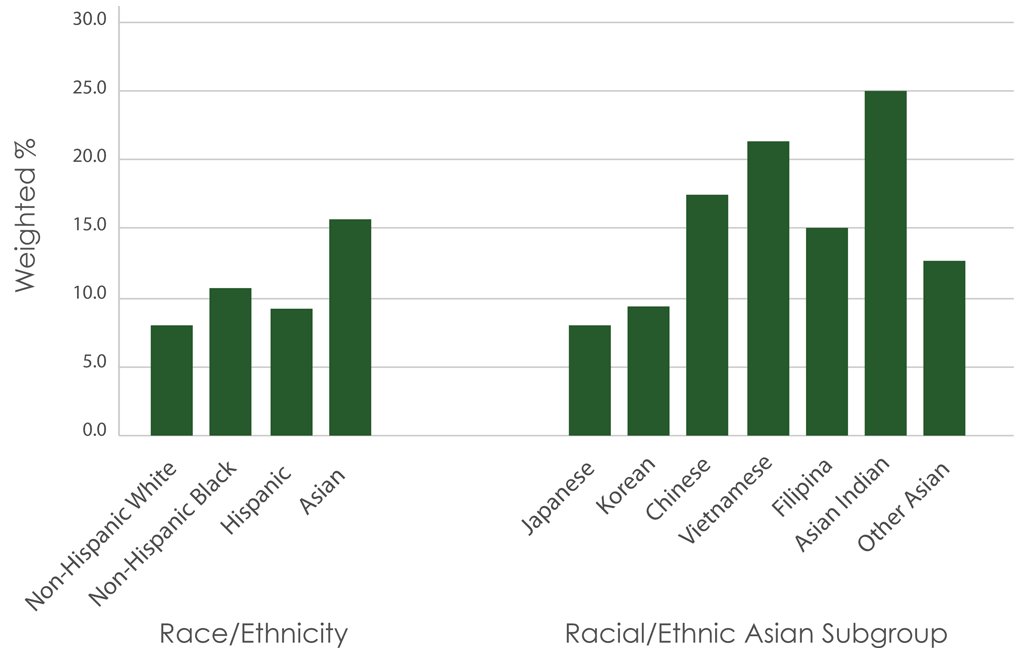
In a study done by professionals from the Department of Public Health Sciences, out of the 5,562 women who were studied, 15.5% of Asian American women had gestational diabetes. Next in line were 9.0% of non-Hispanic black women, 10.7% of Hispanic women, and 7.9% of non-Hispanic white women. Asian women were 95% more likely to have gestational diabetes than non-Hispanic white women.
This was true regardless of the mother’s age, education, marital status, income, level of prenatal care, BMI before pregnancy, or level of physical activity. All women in this study are from Los Angeles, California, had a live delivery, and did not have pre-pregnancy type I or II diabetes.
It’s important to note, though, that while these risk factors can increase the likelihood of developing diabetes, they don’t guarantee its development. Leading a healthy lifestyle and managing these risk factors can significantly reduce your risk of developing diabetes.
What are the Complications of Diabetes?
Untreated or poorly managed diabetes can lead to various complications affecting different organs and systems in the body. Some common complications of diabetes include:
- Cardiovascular disease: Diabetes increases the risk of heart disease, heart attacks, and strokes.
- Neuropathy: High blood sugar levels can damage the nerves, leading to numbness, tingling, and pain in the hands and feet.
- Nephropathy: Diabetes can damage the kidneys and impair their ability to filter waste from the blood.
- Retinopathy: Elevated blood sugar levels can damage the blood vessels in the retina, leading to vision problems and potentially blindness.
- Foot complications: Nerve damage and poor blood circulation can cause foot ulcers, infections, and, in severe cases, amputation.
- Skin conditions: Diabetes increases the risk of skin infections, such as bacterial and fungal infections.
- Depression and anxiety: Living with a chronic condition like diabetes can take a toll on mental health, leading to depression and anxiety.
- Complications during pregnancy: Gestational diabetes can increase the risk of complications for both the mother and the baby, including premature birth and the development of type 2 diabetes later in life.
Managing diabetes through proper treatment, lifestyle changes, and regular medical check-ups can help prevent or delay the onset of these complications.
What are Diabetes Treatments?
The management of diabetes requires a multifaceted approach involving lifestyle modifications, medication, and regular monitoring. The treatment options vary depending on the type of diabetes.
Type 1 Diabetes treatment
Type 1 diabetes requires lifelong insulin therapy. Insulin can be administered through multiple daily injections or an insulin pump. Regular blood sugar monitoring is essential to adjust insulin doses and maintain optimal control.
Type 2 Diabetes treatment
The management of type 2 diabetes typically involves lifestyle changes, such as adopting a healthy diet and increasing physical activity. In some cases, medication may be prescribed to help lower blood sugar levels. Oral medications, injectable medications, and insulin may be used, depending on the individual’s needs.
Gestational Diabetes treatment
As with Type 2 Diabetes, gestational diabetes is managed primarily through lifestyle modifications, including a balanced diet and regular physical activity. Blood sugar monitoring is important to ensure that blood sugar levels are within the ideal range. In some cases, insulin may be necessary to control and maintain blood sugar levels.
If you have diabetes, it’s important for you to talk to your healthcare provider and develop a personalized treatment plan that addresses your specific needs and goals. To know more about insulin, medicines, and other diabetes treatments, check out this information presented by the National Institute of Diabetes and Digestive and Kidney Diseases.
What’s the Recommended Diet for Diabetes?
Diet plays a crucial role in managing diabetes. A healthy eating plan can help control blood sugar levels, promote weight management, and reduce the risk of complications. Here are some dietary considerations for diabetes:
Carbohydrate (Carb) Counting
Carbohydrate counting is a common strategy for managing blood sugar levels in people with diabetes. Monitoring and controlling the intake of carbohydrates can help prevent blood sugar spikes. Choosing complex carbohydrates, such as whole grains, fruits, and vegetables, over simple carbohydrates, such as refined sugars and processed foods, is recommended.
Most people with diabetes aim to get around 50% of their daily calories from carbohydrates. This means that if you consume 1,600 calories per day, for instance, carbohydrates should account for 800 of them. Each gram of carbohydrate contains 4 calories, so you would require approximately 200 grams of carbohydrate per day.
The primary goal of carbohydrate counting is to maintain stable blood glucose levels by dividing your total daily carbohydrate intake evenly between meals. For more effective meal planning, you can check out our Nutrition Database and Calorie Count guide. It provides complete information on the nutrition facts of all foods you plan to eat.
Now when tracking carb consumption, some experts recommend using net carbohydrates as your basis instead of keeping track based on total carbohydrates. To calculate net carbohydrates, you can do it by subtracting dietary fiber and/or alcohol sugar (if there is) from the total carbohydrates indicated. The image below illustrates how to calculate net carbohydrates.

Though this information is useful when keeping track of your carbohydrate intake, it’s important to take note that the current American Diabetes Association (ADA) guidelines have not recommended a specific percentage of ideal carbohydrate intake for people with diabetes. The ADA now advocates for an individualized approach, emphasizing the need to tailor carbohydrate intake and any diabetes diet plan to individual dietary preferences and goals. This is a more rewarding and realistic approach in the long run. You should talk with your healthcare provider first before adjusting anything in your diet.
Balanced Meals
Eating balanced meals that include a combination of carbohydrates, proteins, and healthy fats can help regulate blood sugar levels. Including sources of lean protein, such as poultry, fish, and legumes, along with fiber-rich foods, can help slow down the absorption of carbohydrates and prevent rapid blood sugar fluctuations.
Portion Control
Controlling portion sizes is essential for managing blood sugar levels and weight. Eating smaller, more frequent meals throughout the day can help prevent blood sugar spikes and promote better glycemic control.
Foods to Avoid
People with diabetes should limit or avoid certain foods. These include sugary beverages, processed snacks, high-fat foods, and foods with a high glycemic index. It’s important to read food labels and choose low-sugar, low-sodium, and low-fat options whenever possible.
Working with a registered dietitian who specializes in diabetes management can provide you with more personalized guidance and meal planning strategies that meet your preferences.
What are the Ideal Exercises for Diabetes?
Regular physical activity is an integral part of diabetes management, as it helps improve insulin sensitivity, manage weight, and reduce the risk of complications. Here are some key points to consider when exercising:
Aerobic Exercise
Engaging in aerobic exercises, such as brisk walking, swimming, cycling, or dancing, for at least 150 minutes per week can help improve cardiovascular health and regulate blood sugar levels. It’s important to start slowly and gradually increase the intensity and duration of exercise to avoid overexertion.
Strength Training
Incorporating strength training exercises, such as weightlifting or resistance training, into the exercise routine can help build muscle strength and improve insulin sensitivity. It’s recommended to perform strength training exercises at least twice a week, targeting major muscle groups.
Flexibility and Balance Exercises
Including flexibility and balance exercises, such as yoga or tai chi, can help improve overall mobility and reduce the risk of falls. These exercises can be incorporated into the exercise routine a few times a week.
Blood Sugar Monitoring
Monitor blood sugar levels before, during, and after exercise to ensure that blood sugar levels remain within the ideal range. Adjustments in medication or carbohydrate intake may be necessary based on blood sugar readings.
Before starting an exercise program, individuals with diabetes should consult with their healthcare provider to ensure that it is safe and suitable for their specific condition.
Safety Precautions
People with diabetes should take certain precautions when exercising, such as wearing appropriate footwear, staying hydrated, and carrying a source of fast-acting carbohydrates in cases of low blood sugar (hypoglycemia).
Before starting an exercise program, it’s important to consult with your healthcare provider to make sure that exercise is safe and appropriate for your case.
What Tests Are Used to Diagnose Diabetes?
Early diagnosis of diabetes is important for effective management and the prevention of complications. The following diagnostic tests are commonly used to diagnose diabetes:
Fasting Plasma Glucose (FPG) Test
The FPG test measures blood sugar levels after an overnight fast. A fasting blood sugar level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions indicates diabetes.
A1C Test
The A1C test provides an average of blood sugar levels over the past three months. An A1C level of 6.5% or higher on two separate tests indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
During an OGTT, blood sugar levels are measured after consuming a sugary drink containing 75 grams of glucose. A blood sugar level of 200 mg/dL or higher after two hours indicates diabetes.
Gestational Diabetes Diagnosis
Pregnant women are typically screened for gestational diabetes between the 24th and 28th weeks of pregnancy. The glucose challenge test and glucose tolerance test are commonly used to diagnose gestational diabetes.
If you suspect you may have diabetes or are at risk, it’s important to consult with a healthcare provider for proper testing and diagnosis.
How to Prevent Diabetes?
As mentioned throughout this guide, lifestyle changes can help prevent or delay the onset of diabetes. The following prevention strategies are beneficial, particularly if you’re among those who are at risk of diabetes:

Healthy Eating
Adopting a balanced diet that includes whole grains, fruits, vegetables, lean proteins, and healthy fats can help maintain a healthy weight and regulate blood sugar levels. Limiting the intake of sugary beverages, processed foods, and high-fat foods is also important.
Regular Physical Activity
Engaging in regular physical activity for at least 150 minutes per week can help improve insulin sensitivity and maintain a healthy weight. Finding activities that are enjoyable and incorporating them into daily routines is key to long-term adherence.
Weight Management
Maintaining a healthy weight or losing excess weight can significantly reduce the risk of developing type 2 diabetes. A combination of healthy eating, regular physical activity, and portion control can help achieve and maintain a healthy weight.
Blood Sugar Monitoring
Monitor blood sugar levels regularly to identify any changes and take appropriate action. Lifestyle modifications, such as dietary changes and increased physical activity, can help prevent or delay the progression of diabetes.
Regular Check-ups
Regular check-ups with healthcare providers can help monitor blood sugar levels, assess your overall health, and identify any early signs or risk factors for diabetes. Routine screenings, such as blood tests and blood pressure measurements, are essential for early detection and intervention.
Frequently Asked Questions
1. Is a blood sugar of 120 mg/dL bad?
Yes. If your level is between 100 and 125 mg/dL (5.6 and 6.9 mmol/L), you have prediabetes. This puts you at higher risk of type 2 diabetes, so talk to your healthcare provider about it. A blood sugar level of 126 mg/dL (7 mmol/L) or greater is typically indicative of diabetes.
2. If it’s sugar-free, can I eat as much as I want?
Sugar-free foods can be part of a healthy meal plan, but it’s important to exercise caution. Some sugar-free products contain alternative sweeteners like sorbitol, isomalt, and mannitol, which can still affect your blood glucose levels. Additionally, many sugar-free foods may contain calories, carbohydrates, and high levels of fat. Always read the nutrition labels carefully.
3. What is an A1c?
The A1c test measures your average blood sugar levels over a two-to-three-month period. It provides valuable information about how well you are managing your diabetes. The American Diabetes Association (ADA) recommends an A1c level of less than 7% to minimize the risk of complications.
4. Can prediabetes go away?
Yes. Prediabetes can often be reversed if caught early and simple lifestyle changes are made, like eating better and exercising more. Plus, the changes you make to reverse prediabetes and stop it from turning into type 2 diabetes can also make you healthier overall.
Don’t Hesitate to Reach Out for Help
While a diabetes diagnosis can be a life-altering event, it doesn’t mean you can’t live a fulfilling and healthy life. By understanding “what is diabetes” and knowing its causes, types, treatment, and prevention, you can take proactive steps to reduce your risk and effectively manage diabetes if you’re diagnosed. Managing diabetes requires consistent care and diligence. Over time, you’ll gain a better understanding of how to manage this condition.
Remember to regularly consult your healthcare provider. Managing diabetes involves a team effort, and you’ll need the support of medical professionals, friends, and family. Don’t hesitate to reach out to them if you need help.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
17 sources Expanded:
- National Diabetes Statistics Report. Centers for Disease Control and Prevention. (2023). https://www.cdc.gov/diabetes/data/statistics-report/index.html
- What Is Diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. (2023). https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
- Types of Diabetes. Diabetes UK
https://www.diabetes.org.uk/diabetes-the-basics/types-of-diabetes - Chen L, Shi L, Zhang D, Chao SM. Influence of Acculturation on Risk for Gestational Diabetes Among Asian Women. Prev Chronic Dis 2019;16:190212.
https://www.cureus.com/articles/179352-the-impact-of-using-carbohydrate-counting-on-managing-diabetic-patients-a-review#!/ - Diabetes Complications. American Diabetes Association.
https://diabetes.org/about-diabetes/complications - Good to Know: Diabetes Symptoms and Tests. (2020). Clinical diabetes: a publication of the American Diabetes Association, 38(1), 108.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6969655/ - What is DKA (diabetic ketoacidosis)? Diabetes UK
https://www.diabetes.org.uk/guide-to-diabetes/complications/diabetic_ketoacidosis - American Diabetes Association Professional Practice Committee; 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2022. Diabetes Care 1 January 2022; 45 (Supplement_1): S60–S82.
https://diabetesjournals.org/care/article/45/Supplement_1/S60/138923/5-Facilitating-Behavior-Change-and-Well-being-to - Insulin, medicines, and other diabetes treatments. National Institute of Diabetes and Digestive and Kidney Diseases. (2023).
https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments - H Ibrahim, S. M., Shahat, E. A., Amer, L. A., & Aljohani, A. K. (2023). The Impact of Using Carbohydrate Counting on Managing Diabetic Patients: A Review. Cureus, 15(11), e48998. https://www.cureus.com/articles/179352-the-impact-of-using-carbohydrate-counting-on-managing-diabetic-patients-a-review#!/
- Carb Counting and Diabetes. American Diabetes Association.
https://diabetes.org/food-nutrition/understanding-carbs/carb-counting-and-diabetes - Diabetes Diet, Eating, & Physical Activity. National Institute of Diabetes and Digestive and Kidney Diseases. (2023).
https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity - Palermi S, Iacono O, Sirico F, et al. The complex relationship between physical activity and diabetes: an overview. J Basic Clin Physiol Pharmacol. 2021;33(5):535-547. Published 2021 Sep 29. https://pubmed.ncbi.nlm.nih.gov/34592073/
- Mathew TK, Zubair M, Tadi P. Blood Glucose Monitoring. [Updated 2023 Apr 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555976/
- Understanding A1C Test. American Diabetes Association.
https://diabetes.org/about-diabetes/a1c - Blood sugar test. MedlinePlus. National Library of Medicine. (2023).
https://medlineplus.gov/ency/article/003482.htm - Prediabetes – Your Chance to Prevent Type 2 Diabetes. Centers for Disease Control and Prevention. (2022).
https://www.cdc.gov/diabetes/basics/prediabetes.html




