Medically Accredited
What is Rheumatoid Arthritis Disease: Causes, Symptoms, Treatment, and More
Rheumatoid arthritis disease (RA) is a chronic autoimmune condition that affects the joints. While a cure is not available for RA, treatment may still work when it’s diagnosed early, so it’s important to learn the signs. Read on to learn more about RA, from symptoms to remedies, diets, and other treatments.
What is Rheumatoid Arthritis Disease?
Rheumatoid arthritis (RA) is an autoimmune disease that mainly attacks your joints. It is characterized by the immune system mistakenly targeting the lining of your joints, known as the synovium, causing inflammation, pain, and swelling. Imagine your immune system consistently attacking the tissues in your joints as if they were a threat, and that’s the reality of RA. It’s a battle from within, where your body’s defenses turn against you, causing discomfort and mobility challenges.
This condition is chronic and can affect multiple joints in your body, often with symmetry. So, if one of your knees is affected, most likely the other one will be too.

Inflammation from RA can lead to joint damage or bone erosion if left untreated, so knowing the early signs of RA and seeking treatment as soon as possible is important for you to effectively manage this disease.
What are the Symptoms of Rheumatoid Arthritis?
RA is a chronic disease characterized by symptoms of joint inflammation and pain. These symptoms can come and go, though. There are periods known as flares where these signs and symptoms get worse. On the other hand, there are times when the symptoms disappear completely, and these periods are known as remission.
RA symptoms usually affect the joints in the hands, wrists, and knees. However, they can also extend to various tissues and organs in the body, such as the lungs, heart, and eyes.
Joint Pain and Swelling
As mentioned, you’ll likely notice joint pain and swelling with RA. It’s usually common to feel discomfort in your wrists, hands, knees, and feet. The swelling results from the joint inflammation, which can lead to:
- Morning stiffness that lasts for several hours.
- Painful sensation when you move your joints.
Systemic Symptoms (affecting the whole body)
RA isn’t just about aching joints—it affects your entire body as well. You may experience:
- Extreme Fatigue
- Low-grade fever, indicating inflammation.
- Loss of appetite
- Weakness
These symptoms can make you feel unwell, and they can disrupt your daily routines.
Rheumatoid Nodules and Skin Changes

With RA, you may develop rheumatoid nodules, which are firm lumps that usually form near joints affected by RA. These nodules can range in size and are often found at pressure points of the body, such as the elbows and heels. Also, you may notice that your skin is thinning and you bruise easily.
What are the Causes and Risk Factors for Rheumatoid Arthritis?
In figuring out what might tip the scales toward developing RA, researchers look at both your genetic makeup and the environment or lifestyle you have. Your genes don’t guarantee you’ll get it, but they can increase your susceptibility. Additionally, how you live and interact with your environment can be factors that trigger this disease.
Genetics
You’ve heard the term “it’s in your genes!” right? Well, when it comes to RA, your family history is a piece of the puzzle. Certain genes, like those related to the immune system, can make you more likely to develop the condition. If someone in your family has RA, the likelihood of you developing it as well is higher.
- Family History: A first-degree relative with RA increases your risk.
- Genetics: If you are born with certain genes, called HLA class II genotypes, you are at risk of developing RA.
Environmental Triggers and Lifestyle
The world around you and how you live also have a say in this. Some environmental and lifestyle factors can act as triggers for your immune system to start attacking your joints.
- Smoking: Lighting up is a no-go; it’s one of the most significant environmental risk factors.
- Age and Sex: RA is more common as you age, with most cases appearing between ages 30 and 60. Moreover, RA tends to favor females, who are diagnosed with the condition more often than males. In fact, according to World Health Organization (WHO) statistics, about 70% of people living with RA are female.
- Obesity: High body mass may also increase the risk of developing RA.
- Diet: High consumption of sugar, sodium, and red meat may increase the risk of developing RA.
Given the risk factors above, it’s important to note that RA is an autoimmune disorder, and the exact cause of it remains unknown to this day.
How to Diagnose Rheumatoid Arthritis?
To accurately diagnose RA, your healthcare provider will conduct an assessment that involves a combination of physical examinations, laboratory tests, and imaging techniques. These approaches aim to detect signs of inflammation and antibodies indicative of RA.
Physical Examinations
Your healthcare provider will start with a thorough physical exam, checking for swelling, redness, and warmth in your joints. They’ll assess your joint function to identify any problems with range of motion or strength. This hands-on approach gives your healthcare provider insights into your symptoms and their severity.
Blood Tests
Blood tests are vital in detecting RA. Your healthcare provider will look for the following:
- An elevated erythrocyte sedimentation rate (ESR or sed rate) or C-reactive protein (CRP), which can indicate the presence of an inflammatory process in your body.
- The presence of rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. A high level of these antibodies indicates a higher likelihood of RA.
Imaging Techniques
Imaging techniques give your healthcare provider a closer look at what’s happening in your joints. These can include:
- X-rays: Can reveal joint damage and erosion that is typical of advanced RA.
MRI (Magnetic Resonance Imaging) and ultrasound: Are more sophisticated techniques than X-rays and can find early indications of RA-caused joint damage. They provide detailed images, helping to spot inflammation and guide treatment plans.
What’s the Treatment for Rheumatoid Arthritis?
The treatment of RA focuses on alleviating symptoms, slowing disease progression, and improving your quality of life. It involves a combination of medication, physical therapy, and possible surgical interventions. Here are some ways to manage RA:
Medications
Medications are the go-to for keeping your RA in check. Methotrexate is a common choice and often the first line of defense. It can reduce pain and prevent long-term damage to your joints. You might also use steroids to quickly control flare-ups; they’re great at reducing inflammation but come with side effects if used long-term.
These medications below can slow RA’s progression and may even help send it into remission.
- Conventional DMARDs (Disease-Modifying Antirheumatic Drugs)
- Methotrexate (most common)
- Hydroxychloroquine
- Sulfasalazine
- Biologic DMARDs(works faster than conventional)
- TNF inhibitors
- Interleukin-6 inhibitors
- JAK Inhibitors (JAKi)
- Tofacitinib
- Baricitinib
Biologic DMARDs versus JAK Inhibitors
In a study conducted by the Korean Association of Internal Medicine, it was shown that JAK inhibitors are not inferior when it comes to their effectiveness in treating RA. The chart below shows the comparative effectiveness of both types of medications.
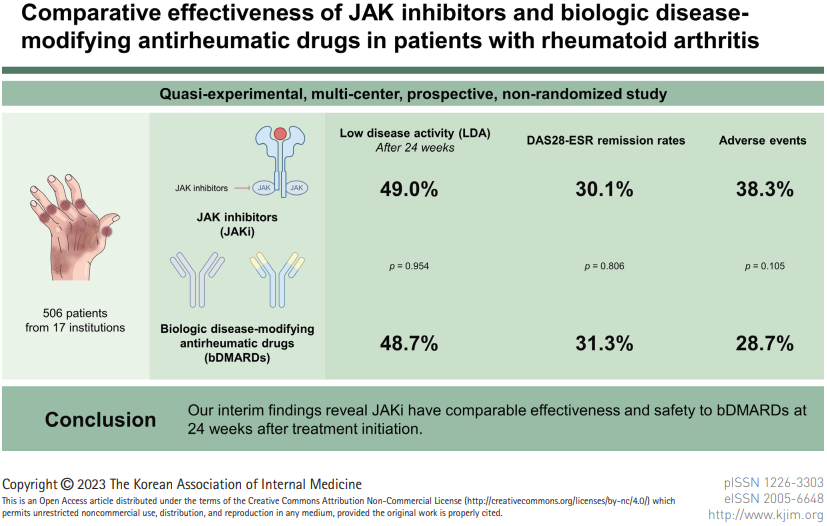
Among the 506 enrolled patients, 346 (196 JAKi group and 150 bDMARD group) were included in the analysis.
After 24 weeks of treatment, 49.0% of JAKi users and 48.7% of bDMARD users achieved LDA (low disease activity)—not much difference. Also, RA remission rates were comparable between those who used JAKi and bDMARDs; rates were 30.1% and 31.3%, respectively. The only difference between the two is the AEs (adverse events) rates, which refer to the adverse reactions linked to the medication. Those who used JAKI had 38.3% AEs, which is higher than the 28.7% AEs exhibited by those who used bDMARDs.
Surgical Interventions
Sometimes, when medication isn’t enough to manage the warmth and pain in your joints, surgery could be an option. These procedures below can fix damaged joints or replace them entirely.
- Synovectomy: Removal of the inflamed lining (synovium) of the joint.
- Tendon Repair: Involves fixing the tendons around your joint that rheumatoid arthritis may have loosened or damaged.
- Joint Fusion: Stabilizing a joint to reduce pain when a joint replacement isn’t an option.
- Total Joint Replacement: Replacing damaged parts of the joint with metal and plastic parts.
Remember, each of the surgical options above comes with risks and benefits that you’ll want to discuss with your healthcare provider.
Physical Therapy
Physical therapy is important for maintaining your joint flexibility and strength. A therapist will guide you through exercises tailored to reduce tenderness and improve the function of your affected joints. They’ll also show you how to use assistive devices if necessary. The physical therapy routine can include:
- Stretching exercises to maintain flexibility.
- Strengthening workouts to keep your muscles strong.
- Hot and cold treatments to manage joint pain and stiffness.
What are Home Remedies for Rheumatoid Arthritis?
Managing rheumatoid arthritis disease (RA) symptoms can significantly change your daily routine. It requires adjustments in how you approach everyday tasks and involves finding ways to maintain joint function and manage symptoms like inflammation and pain.
Daily Life Adjustments
Your day-to-day might look different as you find ways to deal with the fatigue and joint pain associated with RA. Here are some of the adjustments or remedies you can have at home.
- Plan Your Day: On days when you experience a flare, having a plan can make things easier. Break tasks up to avoid overexertion and get enough rest, especially during flare-ups.
- Modify Your Home: Simple modifications like lever door knobs or pull-out shelves can minimize stress on your joints. You can also install grab bars and handrails in bathrooms and on staircases.
- Try Assistive Devices: Braces and splints can be used to keep your joints in a resting position. This may help reduce inflammation, but it is critical to take breaks from using them to avoid “frozen joints” (contractors). Additionally, canes and crutches can help you stay mobile, even during flare-ups.
- Apply hot and cold treatments: Ice packs or warm and cold showers may help to reduce inflammation, pain, and stiffness of joints and muscles.
Exercise and Maintaining Joint Function
Staying active has a crucial role in managing RA, but it’s essential to choose the right type of exercise to avoid putting extra stress on your joints. Here are some of the exercises that’s ideal for you:
- Low-Impact Activities: Activities like swimming or cycling can increase muscle strength around your joints without causing additional impact.
- Flexibility Exercises: Gentle stretching or yoga helps maintain your range of motion and can reduce stiffness.
What are the Complications of Rheumatoid Arthritis?
RA not only affects your joints. It’s an inflammatory disease, and inflammation can spread to your major organs.
- Heart: Your risk of heart disease might go up because RA can affect your heart’s lining and arteries.
- Lungs: Lung issues, like inflammation and scarring, aren’t uncommon with RA, potentially leading to lung disease.
- Kidneys: Inflammation and medication used for RA can sometimes impair kidney function.
- Eyes: Dry eyes and inflammation can occur, which, if not managed, could lead to vision problems.
- Blood Vessels: Blood vessel inflammation can increase the risk of blockages or aneurysms.
- Nerves and Muscles: RA might cause nerve damage and muscle weakness.
To manage these potential complications of having RA, it’s important to have regular checkups with your healthcare provider.
What’s the Difference Between Osteoarthritis and Rheumatoid Arthritis?
Osteoarthritis(OA) and rheumatoid arthritis (RA) are both long-term conditions that affect your bones, and they have similar symptoms. However, knowing the difference helps you understand your symptoms and treatment options better. Keep in mind, though, that it’s possible to have both RA and OA at the same time, which could complicate your treatment, so it’s important to consult with your healthcare provider on this.
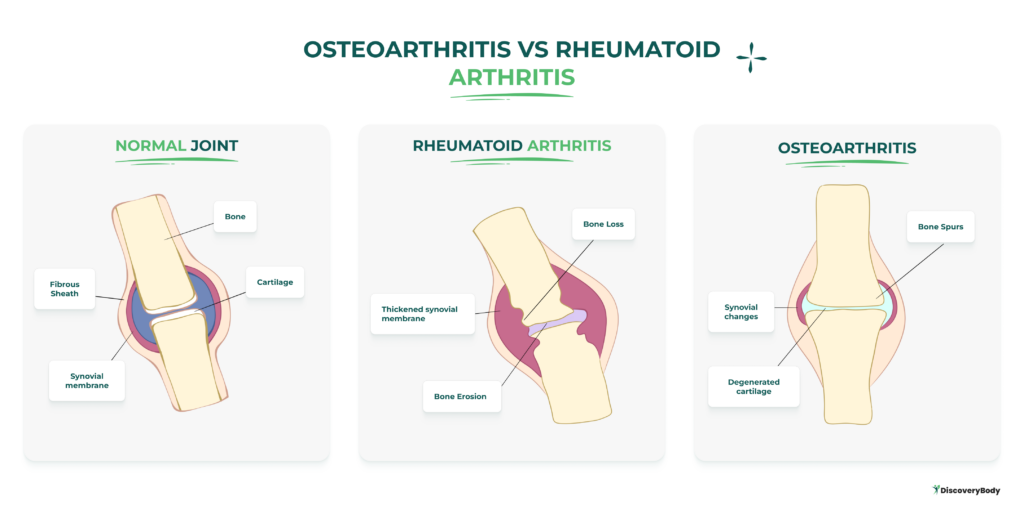
Below is a quick comparison of the two conditions:
| Osteoarthritis (OA) | Rheumatoid Arthritis (RA) | |
|---|---|---|
| Cause | Degenerative joint disease from wear and tear. | Autoimmune disease, where the immune system attacks the lining of joints. |
| Often influenced by aging, joint injuries, obesity, and genes. | Causes involve a mix of genetic and environmental factors. | |
| Symptoms | Joint pain, stiffness, and reduced range of motion. | Joint pain, swelling, and morning stiffness can affect multiple joints. |
| Common in weight-bearing joints (knees, hips, and spine). | Affects small joints in hands, wrists, and feet; can be symmetrical. | |
| Inflammation | Some inflammation, secondary to cartilage degeneration. | Inflammatory arthritis, inflammation central to disease progression. |
| Joint Involvement | Specific joints; often asymmetric. | Multiple joints simultaneously; tends to be symmetrical. |
| Commonly involves weight-bearing joints. | Affects small joints, hands, wrists, feet. | |
| Treatment | Focus on managing symptoms and improving joint function. | Aim to reduce inflammation and prevent joint damage. Medications, therapy. |
| Lifestyle changes, physical therapy, and pain medications. | Disease-modifying drugs, biologics, physical therapy, and lifestyle changes. | |
| Surgical intervention | Surgical intervention |
What are the types of Rheumatoid Arthritis?
RA manifests in various types, each with its own unique characteristics. Knowing which type you have may help you get the treatment that’s best for you. Types of RA include:
Seropositive Rheumatoid Arthritis
If you have seropositive RA, it means your blood tests show the presence of anti-cyclic citrullinated peptides (anti-CCPs) or rheumatoid factors. These antibodies suggest a tendency toward more aggressive forms of the disease. You may experience a wider range of symptoms, including joint damage and inflammation in other parts of your body.
Seronegative Rheumatoid Arthritis
In seronegative RA, your blood does not contain these specific antibodies. Your diagnosis is based on your symptoms, clinical signs, and imaging results. Being seronegative can sometimes make diagnosis more difficult, but it doesn’t necessarily mean a milder form of RA; your symptoms can still be significant and require treatment.
Juvenile Rheumatoid Arthritis
Juvenile Rheumatoid Arthritis (JRA), known as Juvenile Idiopathic Arthritis (JIA), is the most common type of arthritis in children under the age of 17. JRA causes persistent joint inflammation, pain, and swelling that can result in lasting damage to the joints.
Types of JRA:
- Systemic JRA: Affects the entire body; you may experience fevers and rashes along with joint pain.
- Oligoarticular JRA: Affects four or fewer joints, typically larger ones like knees or ankles.
- Polyarticular JRA (RF positive or RF negative): Involves five or more joints and may be associated with a higher risk of having adult rheumatoid arthritis.
What’s the Diet for Rheumatoid Arthritis?
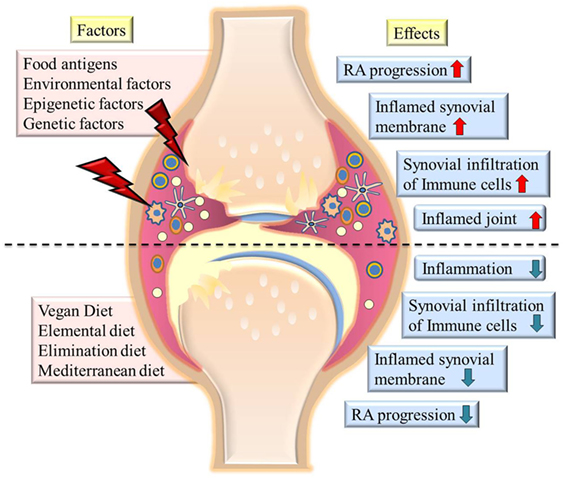
SOURCE: Managing Rheumatoid Arthritis with Dietary Interventions. Khanna S, et al. (2017)
The research supported the impact of dietary changes, specifically the addition of anti-inflammatory foods, on the effective management of RA symptoms. It can help delay disease progression, reduce joint damage, and eventually decrease the dose of medications administered for the therapeutic treatment of patients.
The upper half of the image above shows highly inflamed joints and synovial membrane and increased infiltration of immune cells in joints on exposure to environmental factors or food antigens. The lower half of the image shows the effect of various diets on reducing inflammation, immune cell infiltration, and the severity of RA.
Anti-Inflammatory Foods
Incorporating anti-inflammatory foods into your meals helps fight the inflammation that causes joint pain and stiffness. Add plenty of:
- Fruits and Vegetables: Berries, cherries, and leafy greens are high in antioxidants.
- Whole Grains: Brown rice and oatmeal support steady blood sugar levels.
- Healthy Fats: Olive oil and avocados contain monounsaturated fats, while walnuts and flaxseeds offer omega-3 fatty acids.
If you’re struggling with loss of appetite, which can be common in RA, try small, nutrient-dense snacks that pack in anti-inflammatory benefits.
Dietary Supplements
While your diet should be your main source of nutrients, these supplements may help fill any gaps:
- Fish Oil: High in omega-3 fatty acids, it can help reduce joint inflammation.
- Iron: An iron supplement might be necessary if you have iron-deficiency anemia, a condition often associated with RA.
- Vitamin D: Essential for calcium absorption and bone health.
Before taking any supplements, though, consult with your healthcare provider to make sure they’re suitable for you and won’t have adverse effects when taken together with your medications.
Avoid Trigger Foods
While responses to specific foods differ for everyone, some people with RA find that certain foods worsen the symptoms. Taking note of these trigger foods may help you manage the inflammation and pain associated with RA.
- Processed Foods and Sugars: Usually high in calories and low in nutrients, processed foods and sugars can cause inflammation. Here’s what you need to avoid:
- Refined sugars: Found in soft drinks, candies, pastries, and many pre-packaged snacks.
- Processed snacks: Chips, cookies, and ready meals containing trans fats and preservatives.
- Red Meat and Fried Foods: These contain high-saturated fats that can trigger inflammation. Reduce your consumption of beef, pork, and anything fast food like french fries, burgers, fried chicken, and more.
- Dairy Products: Avoid or limit milk, cheese, and butter.
- Gluten: A protein found in wheat, barley, and rye, may cause adverse immune responses in some individuals with RA. Research suggests that gluten can lead to increased inflammation for those with gluten sensitivity or celiac disease. If you have RA, paying attention to how your body responds to gluten-containing foods is essential, and you might consider getting tested for celiac disease.
- Nightshade Vegetables: Some with RA find that vegetables from the nightshade family, such as tomatoes, peppers, and eggplants, worsen the symptoms. However, this varies among individuals, and not everyone with RA is sensitive to nightshades.
Frequently Asked Questions
- Is there a cure for rheumatoid arthritis?
- Currently, there’s no cure for RA. However, treatments can significantly reduce inflammation, ease symptoms, and slow the progression of the disease.
- What triggers rheumatoid arthritis?
- RA is considered an autoimmune disease and can be triggered by a combination of genetic and environmental factors like infections or smoking, although the exact cause remains unknown
- What are the stages of rheumatoid arthritis?
- The progression of RA usually starts with symptoms like joint pain and stiffness. It can then advance to the swelling of multiple joints, increased pain, and potential joint damage and erosion over time.
- Is there a ‘best’ pain reliever for rheumatoid arthritis discomfort?
- The ‘best’ pain reliever differs for everyone, but NSAIDs, steroids, and DMARDs are commonly used to manage rheumatoid arthritis pain and inflammation. A healthcare provider might also recommend biologic agents or JAK inhibitors.
- What are some unusual signs that might suggest someone has rheumatoid arthritis?
- Unusual signs of rheumatoid arthritis include eye redness and pain, dry mouth, gum irritation, or the feeling of a pebble in your shoe, which could indicate joint issues in your feet.
Talk to your Healthcare Provider
Rheumatoid arthritis disease (RA) isn’t just joint pain—it’s a chronic autoimmune condition that needs your immediate attention. If you’re experiencing symptoms like joint stiffness, swelling, or pain in more than one joint or the same joint on both sides of your body, it’s time to contact your healthcare provider.
Living with RA isn’t about enduring pain—it’s about reclaiming your quality of life! So don’t wait it out; early diagnosis and treatment are important to manage this condition.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up to date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
15 Sources Expanded:
- Rheumatoid arthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH). https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- Rheumatoid arthritis. World Health Organization (2023). https://www.who.int/news-room/fact-sheets/detail/Rheumatoid-arthritis
- Risk factors. Centers for Disease Control and Prevention (2019).https://www.cdc.gov/arthritis/basics/risk-factors.htm
- Deane, K., Demoruelle, M., Kelmenson, L., Kuhn, K., Norris, J., & Holers, V. (2017). genetic and environmental risk factors for rheumatoid arthritis. Best Practice & Research Clinical Rheumatology, 31(1), 3-18. https://www.sciencedirect.com/science/article/abs/pii/S152169421730013X?via%3Dihub
- Cho, S., Kim, H., Song, Y., Kim, H., Nam, E., Lee, S., … & Sung, Y. (2023). comparative effectiveness of jak inhibitors and biologic disease-modifying antirheumatic drugs in patients with rheumatoid arthritis. The korean journal of Internal Medicine, 38(4), 546-556. https://kjim.org/journal/view.php?doi=10.3904/kjim.2022.369
- Rheumatoid arthritis treatment. NHS UK. (2019). https://www.nhs.uk/conditions/rheumatoid-arthritis/treatment/
- Arthritis types. Centers for Disease Control and Prevention (2019). https://www.cdc.gov/arthritis/types/index.html
- Freeman J. (2020). ra vs. os which is worse — rheumatoid arthritis or osteoarthritis? https://www.rheumatoidarthritis.org/ra/ra-vs-oa/
- Osteoarthritis. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH) https://www.niams.nih.gov/health-topics/osteoarthritis
- Lb, N., Lillegraven, S., E, L., Aga, A., Olsen, I., Hb, H., … & Haavardsholm, E. (2016). Patients with seronegative ra have more inflammatory activity compared with patients with seropositive ra in an inception cohort of dmard-naïve patients classified according to the 2010 acr/eular criteria. Annals of the Rheumatic Diseases, 76(2), 341-345. https://ard.bmj.com/content/76/2/341
- Juvenile rheumatoid arthritis. John Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis/juvenile-idiopathic-arthritis
- Rose, S. (2018). rheumatoid arthritis – prevention and treatment with a plant-based diet. Orthopedics and Rheumatology Open Access Journal, 13(1). https://juniperpublishers.com/oroaj/OROAJ.MS.ID.555852.php
- Khanna, S., Jaiswal, K., & Gupta, B. (2017). managing rheumatoid arthritis with dietary interventions. Frontiers in Nutrition, 4. https://www.frontiersin.org/articles/10.3389/fnut.2017.00052/full
- Kurkó, J., Besenyei, T., Laki, J., Glant, T., Mikecz, K., & Szekanecz, Z. (2013). genetics of rheumatoid arthritis — a comprehensive review. Clinical Reviews in Allergy & Immunology, 45(2), 170-179. https://link.springer.com/article/10.1007/s12016-012-8346-7
- Babikir, M. and Gaufri, N. (2017). association of fibrinogen, erythrocyte sedimentation rate and c-reactive protein levels with rheumatoid arthritis. Oalib, 04(04), 1-8. https://doi.org/10.4236/oalib.1103430




