Health, Joint Health
Why Do Your Knees Hurt When Bent?
Knee pain can be caused by a variety of factors other than an underlying disease. Common reasons of knee discomfort include trauma, overuse, and overexertion. Many Americans feel knee pain when they bend, which can be frustrating when we don’t know what’s causing it.
According to experts, for every pound we weigh, our knees might be subjected to four to six times that pressure when we bend them and/or place them in a weight bearing position. Bending, climbing stairs, and squatting can all cause pain in certain areas of the knee.
Your knees bend several times during the day. Movement is required for daily activities such as climbing stairs and sitting in a chair. You also bend your knees while performing workouts like squats and lunges.
The wear and tear of daily life can take its toll on your knees. Furthermore, there are various ligaments, tendons, muscles, and bones in the area. If you have an issue with one of these structures, bending your leg may cause knee discomfort.
Some reasons of knee discomfort are modest and treatable with home remedies. Others need medical treatment. Here, we’ll go over the various reasons of knee pain while bending, as well as signals that you should consult a doctor.

Patellofemoral Syndrome
Patellofemoral syndrome, sometimes known as runner’s knee, is a common condition marked by soreness at the front of the knee. While it is commonly associated with sports such as running, climbing stairs, and squatting, its effects can extend beyond athletes and affect people from many areas of life. Understanding its causes, detecting its symptoms, and obtaining proper therapy are all critical elements in successfully managing this condition.
Causes
The patellofemoral joint connects the kneecap (patella) and thigh bone (femur). A variety of variables can contribute to the development of patellofemoral syndrome. One of the most common causes is kneecap misalignment caused by muscle imbalances or anatomical abnormalities in the lower body. Overuse or repetitive stress on the knee joint, which occurs during sports such as running or leaping, can cause discomfort and inflammation. Furthermore, weak thigh muscles, stiffness in the muscles surrounding the knee, and poor biomechanics can all increase the chance of developing this disease.
Symptoms
- Pain during exercising
- Symptoms of knee discomfort include pain when bending the knee, such as when climbing stairs, leaping, or squatting
- Pain after sitting for long periods with the knee bent, such as while watching a movie.
- cracking or popping sounds in the knee when climbing stairs or sitting for an extended period.
Patellofemoral syndrome does not cause the knee joint to lock. This symptom usually indicates another form of damage, such as a meniscus tear.
Treatment
The treatment for patellofemoral syndrome seeks to reduce pain, address underlying causes, and avoid recurrence. To begin, rest and activity adjustment may be recommended to relieve stress on the knee joint. Physical therapy is essential for strengthening the muscles surrounding the knee, increasing flexibility, and correcting biomechanical abnormalities. Therapeutic activities aimed at the quadriceps, hamstrings, and hip muscles can help restore balance and stability to the knee joint.
Furthermore, chilling, bracing, or taping might provide brief relief from pain and inflammation.
Prevention
To prevent patellofemoral syndrome, keep strong and flexible muscles around the knee joint. Regular strength training activities, stretching routines, and proper warm-up techniques will help lessen the likelihood of acquiring this illness. It’s also important to gradually increase the intensity and duration of physical activity to avoid overloading the knee joint. Using suitable footwear and supportive orthotics can improve stability and cushioning during high-impact exercises.

Patellar Tendonitis
Patellar tendonitis is a common injury or inflammation of the tendon that joins your kneecap (patella) and shinbone (tibia). Your pain could be slight or severe.
Anyone can get patellar tendinitis. But it’s such a common injury among sportsmen, particularly those who play volleyball and basketball, that it’s dubbed jumper’s knee. An estimated 14.4% of recreational volleyball players have jumper’s knee. The frequency is even higher among top professional athletes. According to trusted sources, 40 to 50 percent of elite volleyball players have jumper’s knee.
Continue reading to learn more about why this happens, how to recognize it, and treatment options.
Causes
Patellar tendonitis is caused by repetitive stress on the knee, most commonly due to overuse in sports or activity. The repetitive stress on the knee causes microscopic tears in the tendon, which eventually inflame and weaken it.
Contributing factors can include:
- Tight leg muscles
- Uneven leg muscle strength
- Misaligned feet, ankles, and legs
- Factors to consider include obesity, inadequate padding in shoes, and harsh playing surfaces
- Chronic disorders that weaken tendons
Athletes are especially vulnerable because sprinting, jumping, and squatting exert additional force on the patellar tendon. Running, for example, can exert forces on your knees that are up to five times your own body weight.
Symptoms
Patellar tendonitis symptoms include scorching or severe pain near the base of the kneecap, especially during physical activity such as leaping, running, or squatting. The discomfort may be moderate at first and only occur during or after activity, but if not treated, it can intensify with time. Individuals with patellar tendonitis may experience swelling, soreness, or stiffness around the knee joint. In severe situations, the discomfort may interfere with daily activities, limiting participation in sports or exercise.
Management
Effective care of patellar tendinitis involves minimizing discomfort, facilitating healing, and preventing future damage. Rest and activity modification are critical components of initial treatment, allowing the tendon to recover while lowering stress on the knee joint. Ice therapy can aid with pain and inflammation, and nonsteroidal anti-inflammatory medicines (NSAIDs) can provide brief relief from discomfort.
Physical therapy is an important part of the rehabilitation process, with the goal of strengthening the muscles around the knee, improving flexibility, and correcting any biomechanical abnormalities that are causing the condition. Therapeutic exercises for the quadriceps, hamstrings, and calf muscles can help restore balance and stability to the knee joint while minimizing tension on the patellar tendon. Ultrasound or extracorporeal shockwave therapy can also be used to stimulate tissue repair and relieve pain.
Prevention
To prevent patellar tendinitis, follow proper training techniques, warm-up and cool-down routines, and gradually increase activity intensity and duration. Strengthening the muscles surrounding the knee joint, particularly the quadriceps and hamstrings, with targeted workouts can help lower the risk of stressing the patellar tendon.
Furthermore, wearing appropriate footwear with adequate cushioning and support during physical activity can reduce impact on the knee joint and lower the risk of injury.

Iliotibial (IT) Band Syndrome
What is the IT band?
The iliotibial band (IT band) is also known as the iliotibial tract and Maissiat’s band. It is a lengthy section of connective tissue, also known as fascia, that runs around the outside of your leg from the hip to the knee and shinbone. The IT band helps to extend, abduct, and rotate your hip. It also assists in stabilizing and moving the side of your knee while protecting the outside thigh.
Iliotibial Band Syndrome
The IT band syndrome (ITBS) is a common lateral knee ailment. This sort of injury is typically caused by excessive and repetitive knee flexion and extension. It happens when the IT band gets tight, irritable, or inflamed. When bending, this tightness generates friction on the outside of the knee, causing pain. It can sometimes lead to referred hip discomfort.
Causes
ITBS is caused by excessive friction from an abnormally tight IT band pushing against bone. It is primarily an overuse ailment caused by repetitive actions. ITBS produces friction, discomfort, and pain when moving the knee. It appears to affect only some people, while the reasons for this are unclear.
It’s particularly common among cyclists and runners. It can even occur as a result of walking up and down stairs repeatedly, wearing high heels, or sitting with bent knees for extended periods of time.
The risk factors for getting ITBS are:
- Underlying iliotibial band tension or previous injury
- Weak hip, gluteal, and abdominal muscles
- Walking or running on a track or uphill may result in weakness or lack of flexibility
- Excessive sitting, weak knee extensors, flexors, and hip abductors, together with repetitive activities like jogging and cycling, can lead to knee arthritis
- Unbalanced leg lengths
- Bowlegs and flat feet
Who Gets IT Band Syndrome?
ITBS can affect anyone. It is especially prevalent among runners, cyclists, and hikers. Athletes who use their knees, such as basketball, soccer, and weightlifting, are more likely to develop ITBS.
IT band syndrome is most commonly seen in younger athletes or those who exercise regularly. Often, it is due to training errors that can be remedied.
Training mistakes include:
- Improper warming and cooling might lead to overexertion.
- Excessive physical exertion and insufficient recuperation between workouts
- Wearing inappropriate shoes.
- Training on the incorrect surfaces.
- Improper bicycle fit, rapid training, and bad form are all potential causes of injury.
Treatment Options
ITBS is usually successfully cured and treated with conservative therapy.
Conservative therapies include:
- Using nonsteroidal anti-inflammatory medications (NSAIDs)
- To alleviate symptoms, try icing and relaxing the affected area for the first week, stretching daily, and strengthening muscles, particularly the hips.
- Corticosteroid injections or surgery may be used in really severe, persistent instances. However, you should start with conservative therapy and be consistent.
How to Prevent IT Band Issues
To avoid IT band troubles, you must take care of your body while exercising. Maintain proper form and avoid pushing yourself beyond your capabilities. When working out, always stretch before warming up and cooling down. To loosen up your IT band, consider using a foam roller.
Continue exercising to strengthen and stretch your body. This will also help to balance your body if you frequently engage in the same type of repetitive exercise. Perform the exercises at least three times a week. Take at least one full day of rest per week to allow your body to recover between workouts.

Hamstring Tendonitis
The hamstring muscle group consists of two inner, or medial, muscles. These muscles are called the semitendinosus and semimembranosus. The biceps femoris is an outside, or lateral, muscle. Tendons, a type of connective tissue, connect the muscles to the pelvis, knee, and shinbones, allowing the knee to bend and the hip to extend.
When hamstring tendons are abused or mishandled, small rips form, resulting in irritation and pain.
Hamstring tendonitis can occur laterally or medially, depending on the muscles involved. They can also be defined as distal, including the tendons around the knees, back thighs, and calves.
Tendon inflammation is properly referred to as tendinitis, however the phrases have become synonymous due to widespread use. Tendonitis is frequently confused with tendinosis, which is a chronic disorder caused by repeated usage or injury.
Symptoms of Hamstring Tendonitis
The most prevalent signs of hamstring tendinitis are:
Sharp, scorching pain with muscle and joint weakness.
Symptoms may include:
- aching, dull throbbing, and stiff muscles and joints
- Swelling or inflammation
- Symptoms worsen with additional exercise or use, and they are frequently worse after extended periods of inactivity, such as sleeping or sitting.
Symptoms frequently intensify in the first several hours after injury, then progressively fade. Tight or irritated hamstring tendons frequently produce radiating discomfort in knees, thighs, buttocks, and lower back.
Treatment Options for Hamstring Tendonitis
Most patients find that adopting the RICE approach (rest, ice, compression, and elevation) for 72 hours is sufficient to alleviate symptoms.
Ice causes blood vessels to contract, resulting in decreased blood flow and, consequently, irritation. Ice should be applied for no more than ten minutes at a time. After a 20-minute respite, ice can be administered several times using the same 10-minute on, 20-minute off pattern as before. Icing sessions can be done twice or three times per day.
Compressing and elevating the damaged area reduces inflammation by limiting blood flow to the area.
Over-the-counter nonsteroidal anti-inflammatories such as ibuprofen (Advil, Motrin) and naproxen (Aleve) can help control symptoms in the days following an accident. If the pain lasts longer than a few days or does not respond well to basic treatment, consult a doctor.
Recovery Time and Immediate Treatment Exercises
When wounded tissues are asked to function too quickly, they frequently do not fully recover. Tendons that are weak are much more likely to be re-injured. The more times the same tissue is destroyed, the higher the risk of long-term harm.
It usually takes a few days for patients to feel significant relief, and six weeks or more to feel completely recovered.
For the first 48 hours, avoid doing anything that will trigger the tendon. After then, only undertake workouts that do not cause more pain.
In the first week after an injury, you can begin reintroducing cautious, steady activities that focus on preserving overall strength. Isometric knee flexes are a wonderful place to start. Place the affected hamstring over the opposite leg and contract at 30, 60, and 90-degree angles as comfortable.
Long-term Recovery Exercises
After about a week, you can normally begin range of motion, lengthening, and strengthening exercises. A single-leg windmill makes an excellent starting point. To perform this exercise:
- Rest the uninjured leg on a chair and keep the other straight.
- Reach down with a flat back.
- Hold the stretch for thirty seconds.
- You can use portable weights to make the stretch more difficult.
The Nordic hamstring exercise is another useful stretch.
- Kneel and bend forward as much as is comfortable, keeping your hips neutral.
- Have a helper hold your feet.
- Hold the stretch for thirty seconds.
After a few weeks, you can begin incorporating additional workouts that engage the muscle in a prolonged state. A useful workout is to lie on your back with a bent knee and use an elastic resistance band to provide an opposing force while slowly flexing the knee.
Four to six weeks following the injury, you can begin adding more intense workouts such as squats, hamstring curls, and hamstring bridges. These can help to strengthen the entire region and avoid further injuries.
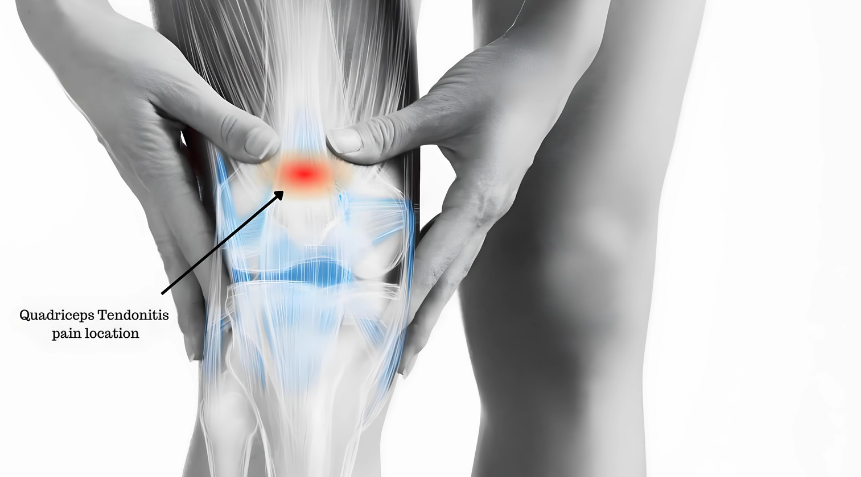
Quadriceps Tendonitis
The quadriceps tendon connects your quadriceps muscles to your kneecap. It works by straightening your knees, which allows you to walk, jump, and climb stairs.
If the tendon becomes inflamed, it is known as quadriceps tendinitis or quadriceps tendonopathy. It can also be spelled tendinitis.
It is commonly caused by repetitive actions such as jumping or kneeling. This misuse causes small tears, resulting in pain and edema.
The injury frequently affects athletes, such as volleyball and basketball players. Quadriceps tendinitis, on the other hand, can affect anyone who exercises regularly. The risk increases if you suddenly increase your physical activity.
Continue reading to learn about the causes and symptoms of quadriceps tendinitis, as well as treatment options.
Symptoms
Quadriceps tendinitis causes pain in the front of the knee, directly above the kneecap. Usually, the pain is dull and gradually worsens with time.
The pain may worsen after prolonged sitting, leaping, squatting, or running.
Some people’s pain may go away during activity only to return after they stop moving.
Additional symptoms include:
- Symptoms include morning stiffness, edema, and pain
- weakness
- Poor mobility
Causes
The most common cause of quadriceps tendonitis is overuse. This occurs when the tendon moves in a precise pattern repeatedly, resulting in tiny tears.
Normally, your body attempts to repair these tears. However, if you keep performing the same movement, additional tears will appear.
Quadriceps tendinitis can be caused by repeated movements, such as:
- Sports-related injuries, such as jumping on a hard surface, can lead to a sudden increase in physical activity.
- Poor posture and walking habits.
Treatments for Quadriceps Tendinitis
Once your doctor has determined the severity of your injury, they will develop a specific treatment plan. Typically, treatment requires a combination of treatments.
Nonsurgical Treatment
Typically, treatment begins with conservative measures. This includes nonsurgical treatments.
RICE
The first-line treatment for quadriceps tendinitis is a technique called RICE. The treatment includes:
- Rest. To protect the afflicted area, avoid overworking your knees. You may require a brace to support your knee.
- Ice. Ice or a cold compress might help reduce swelling and pain.
- Compression. A compression bandage will also help reduce edema.
- Elevation. To reduce swelling even further, elevate your damaged knee.
Physical Therapy
Once the swelling subsides, your doctor may recommend that you see a physical therapist. They can offer therapies such as:
- Massage therapy includes both hot and cold treatments.
- Ultrasound therapy and tailored fitness programs.
Quadriceps Tendonitis Exercises
A physical therapist can demonstrate how to safely perform quadriceps tendinitis exercises.
These exercises target your hamstrings and hips, which help support your knee tendons. They also contain workouts to improve the flexibility of the quadriceps tendon and surrounding muscles.
Tape and Brace for Quadriceps Tendonitis
A physiotherapist or physical therapist may apply athletic tape to your knee to relieve tension on the tendon. Taping alleviates knee pain by stabilizing the kneecap.
Another option is a knee brace, which relieves tension on your tendon.
Orthotics
Orthotic devices are shoe inserts designed to support the foot. They assist cure tendinitis by relieving pressure on the knee tendons.
Depending on your symptoms, your doctor may suggest a store-bought or custom-made orthotic insert.
Anti-inflammatory Drugs
Nonsteroidal anti-inflammatory medications (NSAIDs) are pain relievers available without a prescription. Tendonitis discomfort can be treated with the following nonsteroidal anti-inflammatory drugs:
- ibuprofen
- naproxen
- aspirin
Speak with your doctor about whether it is safe for you to use NSAIDs. Your doctor may recommend acetaminophen instead of an NSAID.
Your doctor may also recommend local corticosteroid injections, which are injected into your knee.
Quadriceps Tendon Surgery Repair
Most persons with quadriceps tendinitis do not require surgery. However, if nonsurgical therapies fail or your injury is serious, you may require surgical surgery.
During surgery, a surgeon will remove the injured piece of your tendon. The surgical possibilities include the following procedures:
- Open surgery requires a single major incision.
- Arthroscopic surgery employs small incisions, a tiny video camera, and miniature surgical instruments. It is less intrusive than open surgery.
- Percutaneous ultrasonic tendon debridement use ultrasonic energy to remove injured tissue.

Bursitis
If you are experiencing joint pain or stiffness, you may be wondering what the underlying cause is. Bursitis and different kinds of arthritis can all cause joint pain.
Arthritis can take various forms, including osteoarthritis (OA) and rheumatoid arthritis (RA). RA is more inflammatory than osteoarthritis.
Bursitis, OA, and RA have certain symptoms, but their long-term prognosis and treatment regimens differ.
Most cases of bursitis can be treated and resolved. Both OA and RA are chronic conditions, while symptoms may be reduced and flared again at times.
Bursitis develops when a fluid-filled sac known as a bursa swells. Bursas provide padding between your joints and are found throughout your body.
Body components include:
- bones
- skin
- muscles
- tendons
You may have bursa inflammation if you participate in an activity that demands repetitive motion, such as a sport, hobby, or manual labor.
Diabetes, crystal deposition (gout), and infections can all cause the disease.
It is typically a transient condition that resolves after a few weeks of treatment. It may return from time to time. It can develop chronic if left untreated or if caused by another condition.
How Can You Tell if it’s Bursitis?
It may be tough to identify the source of your joint pain. You will most likely require a doctor to diagnose your ailment because the short-term symptoms can be very similar.
Bursitis can cause intermittent joint discomfort, whereas chronic pain can be caused by osteoarthritis.
If you experience a sudden onset of symptoms after engaging in a repetitive motion activity such as playing tennis or crawling around on your hands and knees, you should look into bursitis.
RA symptoms may spread to different joints in your body. Joint swelling is common, as are rheumatoid nodules on the skin.
How is it Diagnosed?
To begin diagnosing your disease, your doctor will need to perform a physical examination, explain your symptoms, and obtain a health and family history, whether you have bursitis, OA, or RA.
These basic actions may be sufficient to diagnose bursitis. Your doctor may order laboratory tests to rule out infections, ultrasound to confirm bursitis or tendinitis, or further testing to detect cellulitis.
Imaging and other lab tests are increasingly commonly used to diagnose OA and RA. Your doctor may even prescribe a rheumatologist for evaluation and treatment of these chronic illnesses.
Treatment
This illness can be managed at home using a range of approaches, including over-the-counter (OTC) drugs and doctor or specialist interventions.
The first-line treatment for bursitis may include:
- To treat joint pain and swelling, try applying ice and heat
- resting, exercising, padding sensitive joints
- wearing a brace or splint, and taking over-the-counter medications like ibuprofen and naproxen.
If these therapies do not alleviate your symptoms, your doctor may recommend physical or occupational therapy, stronger oral or injectable prescription drugs, or surgical procedures.
It’s worth noting that surgery is only indicated in exceptional cases.

Osteoarthritis
Osteoarthritis (OA) is a type of degenerative joint pain caused by wear and tear on the joints.
As you age, the cartilage that cushions your joints begins to wear away, causing the bones to grind together. The bone-on-bone action causes inflammation of the joints.
OA mostly affects the joints in your arms and legs, including your fingers, wrists, knees, ankles, and hips.
The lower back is also a common site of OA discomfort. Inform your doctor if you are experiencing the following early symptoms of OA.
Symptoms of Osteoarthritis
Pain
“Oh, my aching back” is a phrase you’ve likely heard before. You may even have said it yourself. Arthritis patients are all too familiar with hurting backs, necks, knees, and hips.
Early arthritis aches can be categorized into two types: pain and tenderness. You may also experience sharper pain while moving your affected joint in a certain way, such as opening a jar with arthritic fingers.
Tenderness
Tenderness is the discomfort you experience when you press down on a joint. Tenderness can sometimes include apparent swelling around the joint, but this is more typical in the latter stages of OA.
Joint Stiffness
Joint discomfort is accompanied with stiffness. Joint stiffness is natural when you wake up or after sitting at your desk all day. It’s also indicative of early OA. That wooden sensation that makes you feel lethargic and slow may make you want to go back to bed, but avoid the temptation. People with arthritis frequently feel better after warming up their joints with some light activity or simply going about their everyday routines.
Abnormal Sensations
Cartilage is intended to act as a shock absorber, allowing your joints to move more smoothly. When cartilage wears down, bone-to-bone rubbing can provide a variety of unusual feelings. Grating of the joints is prevalent among persons with OA. It is the result of the bones rubbing together. When you move, you may feel or hear your joints clicking or crackling.
Loss of Flexibility
People in the early stages of arthritis may discover that moving the affected portions of their body is more difficult than it was previously. Joint stiffness and pain can contribute to loss of flexibility, also known as range of motion. The range of motion refers to the amount to which your joints can move in their typical patterns. For example, your knee’s range of motion includes fully bending and extending. If you have arthritis, you may be unable to bend your knees as far. Loss of flexibility is typically a gradual process.
Timing of Your Discomfort
Pain, discomfort, and joint stiffness are typically limited to certain times in the early stages of osteoarthritis. You may notice that your hips pain after a game of basketball, or that your back feels tight first thing in the morning. As degenerative arthritis advances, you may experience achy joints even while you are at rest.
Management and Solutions
You and your doctor can work together to develop an OA management plan to alleviate arthritis pain. Over-the-counter pain medications, joint bracing, and range-of-motion exercises can all help you stay independent and active.
Baker’s (Popliteal) Cyst
What is a Popliteal Cyst?
A popliteal cyst, also known as a Baker’s cyst, is a fluid-filled swelling that forms a bump at the back of the knee, causing tightness and limited movement. The cyst can cause pain when you bend or extend your knee.
This condition is usually caused by an issue with the knee joint, such as arthritis or a cartilage injury. Treating the root cause can typically resolve the issue. A popliteal cyst can not cause long-term damage, although it can be extremely unpleasant and, in rare cases, explode. Fluid can then travel down the calf, resulting in a “bruise” around the ankle.
Causes
Synovial fluid is a transparent liquid that ordinarily circulates in the chambers of your knee joint. Sometimes the knee produces an excessive amount of this fluid. The growing pressure forces the fluid to the back of the knee via a one-way valve, causing a bulge. This significant swelling of the knee leads to the formation of a popliteal cyst.
The most common causes of popliteal cysts are:
- Damage to the knee cartilage (meniscus)
- Knee arthritis
- Rheumatoid arthritis
- Other joint diseases can produce inflammation
The knee is a complicated joint that can easily be injured. According to the American Academy of Orthopedic Surgeons (AAOS), around 10.4 million Americans saw their doctors in 2010 for a knee ailment, making it the most prevalent cause for consulting an orthopedic specialist. Such injuries may produce inflammation, resulting in a popliteal cyst.
A blood clot may also produce bruising and swelling behind the knee and on the back of the calf. It is critical that your doctor inspect the swelling to identify whether the culprit is a cyst or a clot.
Symptoms
A popliteal cyst may not cause you any pain. In certain circumstances, you might not detect it at all. If you have symptoms, they may include:
- Mild to severe discomfort and stiffness.
- Limited range of motion.
- Symptoms may include swelling behind the knees, bruising, and cyst rupture.
Management and Treatment
Treating a Popliteal Cyst
A popliteal cyst usually does not require treatment and will go away on its own. However, if the swelling becomes too great and causes considerable pain, your doctor may suggest one of the following therapies.
Fluid Draining
Your doctor will inject a needle into the knee joint and may use ultrasound to guide it to the proper location. They will then drain the fluid out of the joint.
Physical Therapy
Regular, gentle workouts will help you improve your range of motion and strengthen the muscles around your knee. Crutches may assist relieve the pain. You can also assist relieve discomfort by applying a compression wrap or ice to the joint.
Medication
Your doctor may prescribe a corticosteroid medicine, such as cortisone. Your doctor will inject this medication into the joint, which will then flow back into the cyst. While it may alleviate pain, it does not always prevent a popliteal cyst from returning.
Treating the underlying cause of the cyst is critical to preventing it from recurring. As a general rule, if the cyst is left alone, it will disappear after the underlying reason is addressed. If your doctor determines that you have cartilage damage, he or she may propose surgery to repair or remove it.
If you have arthritis, the cyst may linger long after your doctor has addressed the underlying reason. If the cyst is causing you pain and limiting your range of motion, your doctor may consider surgery to remove it.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
Sources Expanded
- Why Do My Knees Hurt When Bending? – The Orthopaedic Institute. (2021, September 13). The Orthopaedic Institute. https://www.toi-health.com/physician-articles/why-do-my-knees-hurt-when-bending/#:~:text=Knee%20pain%20when%20bending%20may,a%20clear%20and%20obvious%20cause.
- Nunez, K. (2023, February 3). What Causes Knee Pain When You’re Bending It, and How’s It Treated? Healthline. https://www.healthline.com/health/knee-pain-when-bending#causes
- Huizen, J. (2020, April 30). Everything You Should Know About Hamstring Tendonitis. Healthline. https://www.healthline.com/health/hamstring-tendonitis
- Cronkleton, E. (2018, August 18). IT Band Stretches, Strength Exercises, and More. Healthline. https://www.healthline.com/health/it-band#exercises
- Crna, R. N. M. (2017, August 8). Patellofemoral Syndrome. Healthline. https://www.healthline.com/health/patellofemoral-syndrome#symptoms
- Hecht, M. (2018, September 3). What Is Patellar Tendonitis (Jumper’s Knee)? Healthline. https://www.healthline.com/health/patellar-tendonitis#causes
- Knee Pain When Bending? Here’s What You Can Do About It | Guthrie. (n.d.). https://www.guthrie.org/blog/knee-pain-when-bending-heres-what-you-can-do-about-it
- Nunez, K. (2019, December 10). Causes and Treatments for Quadriceps Tendinitis. Healthline. https://www.healthline.com/health/quadriceps-tendonitis#treatment
- Underwood, C. (2018, September 17). Baker’s (Popliteal) Cyst. Healthline. https://www.healthline.com/health/bakers-cyst#qampa
- Roth, E. (2023, May 24). 6 Early Symptoms of Osteoarthritis (OA): Pain, Tenderness, and More. Healthline. https://www.healthline.com/health/early-symptoms-osteoarthritis
Trusted Health, Wellness, and Medical advice for your well-being