Health Conditions
How Urinary Incontinence May Lead to UTIs
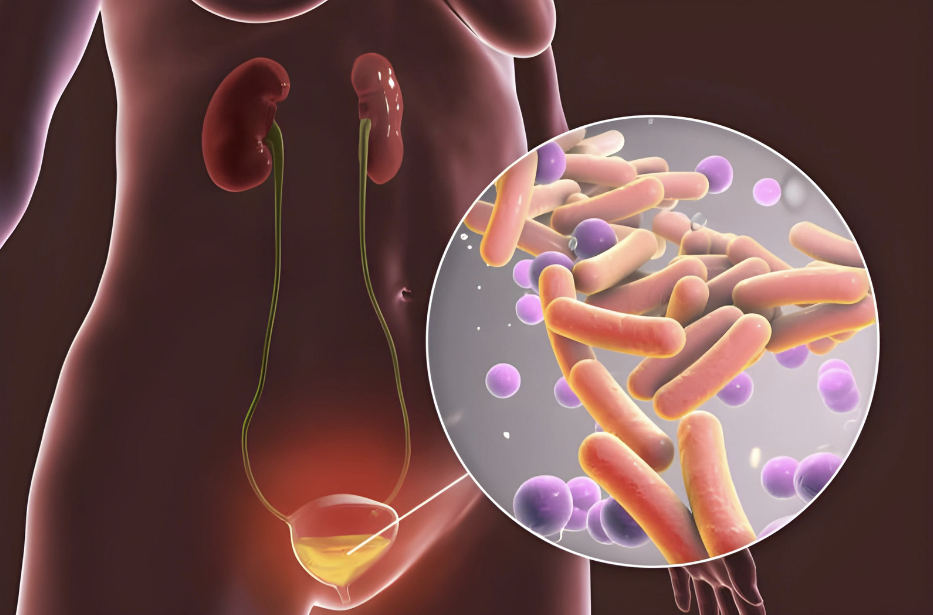
Navigating the complexities of urinary health reveals a maze of interconnected elements, where disorders like urinary incontinence and urinary tract infection (UTIs) frequently collide, posing a challenge for those dealing with these prevalent ailments. Urinary incontinence is defined as the involuntary leakage of urine, whereas UTIs are caused by bacterial colonization within the urinary system.
Despite the agony and difficulty caused by urine incontinence, a serious concern remains: Can this condition predispose people to UTIs? Exploring this complex relationship offers light on the putative processes that link urinary incontinence to UTI formation and emphasizes the significance of comprehensive care options that aim to preserve urinary health while reducing the risk of recurring infections. This article investigates the dynamic connection between urinary incontinence and UTIs, providing insights into potential preventive measures and treatment options to improve urinary function and general well-being.

Understanding Urinary Incontinence and UTIs
Urinary incontinence and urinary tract infections (UTIs) are distinct illnesses, however they may be connected. Urinary incontinence refers to the involuntary flow of urine, whereas UTIs are infections of the urinary tract. In some situations, urine incontinence can result in UTIs, and vice versa.
The Connection Between Urinary Incontinence and UTIs
Urinary incontinence can raise the chance of having a UTI. When pee escapes from the bladder and onto the skin, bacteria can enter the urethra, resulting in an infection. UTIs can also induce urine incontinence, especially in older people. The infection may irritate the bladder, causing it to contract and leak urine involuntarily.
Risk Factors and Causes
There are various risk factors and causes that might lead to urinary incontinence and UTIs. The most prevalent risk factors for urine incontinence are age, menopause, an enlarged prostate, pregnancy, and certain drugs. Bacteria, such as E. coli, often cause UTIs when they enter the urethra and migrate up to the bladder. Women are more prone than males to have UTIs, and some circumstances, such as sexual activity and the use of certain birth control methods, might raise the chance of infection.
Other illnesses, such as diabetes, can increase the likelihood of having urine incontinence and UTI. Diabetes can impair the nerves that control the bladder, resulting in incontinence. It can also deplete the immune system, making it more difficult for the body to combat illnesses.
In conclusion, urine incontinence and UTIs are two distinct disorders that may be connected. Urinary incontinence raises the likelihood of having UTIs, and vice versa. Both diseases can be caused by a variety of reasons, including age, menopause, an enlarged prostate, pregnancy, sexual activity, and certain medical conditions. If you are suffering symptoms of urinary incontinence or a UTI, you should consult with a healthcare specialist to evaluate the underlying cause and the best course of treatment.

Symptoms and Diagnosis
Recognizing Symptoms of UTIs
Individuals with urinary incontinence frequently develop urinary tract infections (UTIs). UTIs can produce a wide range of symptoms, including temporary urine incontinence. Some of the common symptoms of UTIs are:
- A persistent urge to urinate.
- A scorching sensation when urinating
- Urinating frequently, passing little volumes of pee.
- Urine that appears hazy
- Urine that appears crimson, bright pink, or cola-colored: indications of blood in the urine.
- Urine with a strong fragrance
- Pain or discomfort in the lower stomach or back
- Fever, chills, nausea, or vomiting.
It is crucial to realize that not everyone with a UTI develops symptoms. In other circumstances, UTIs are asymptomatic, which means the person is unaware of the infection.
Diagnosing Urinary Incontinence and UTIs
If a person is having symptoms of urinary incontinence or UTIs, they should seek medical assistance. A doctor can do a physical examination and prescribe tests to determine the ailment.
To diagnose urinary incontinence, a doctor may do a urine test to look for evidence of infection or other abnormalities. They may also request that the individual keep a bladder diary, which includes tracking the amount of fluids taken, the frequency of urination, and any instances of urine leakage.
To diagnose a UTI, a doctor may do a urine culture test to detect the presence of bacteria in urine. They may also run a blood test to look for symptoms of infection.
Overall, identifying the symptoms of UTIs and obtaining immediate medical assistance can help people with urine incontinence avoid complications and improve their results.

Treatment and Management
Medical Treatments for UTIs and Incontinence
Medical therapies for UTIs and incontinence are often prescribed by a healthcare practitioner or physician. Antibiotics are widely used to treat UTIs because they help eradicate the germs that cause the illness. Anticholinergics and mirabegron, which can relax bladder muscles and enhance bladder function, may also be recommended to help with incontinence management.
In some circumstances, surgery may be needed to manage incontinence, especially if other treatments have been unsuccessful. Surgical options include bladder suspension surgery, sling techniques, and prosthetic urinary sphincter implants.
Lifestyle and Home Remedies
In addition medication therapies, lifestyle adjustments, and home remedies may help manage UTIs and incontinence. Pelvic floor exercises, such as Kegels, can assist to strengthen and improve bladder control. Dietary adjustments, such as increasing fluid intake and limiting caffeine and alcohol, may also assist manage incontinence.
To avoid future UTIs, increase fluid intake and take vitamin C or cranberry supplements. Good hygiene habits, such as wiping from front to back after using the restroom, can also help prevent UTIs.
Probiotics may also help prevent UTIs by promoting a healthy balance of bacteria in the urinary tract. Women with incontinence caused by vaginal atrophy may potentially benefit from estrogen therapy.
Overall, treating and managing UTIs and incontinence may require a combination of medical treatments, lifestyle changes, and home remedies. It is critical to talk with a healthcare provider or doctor to identify the best course of action for your specific needs.

Prevention and Long-Term Outlook
Preventative Measures
Preventing urinary incontinence is an important step toward avoiding urinary tract infections (UTIs). Individuals can take numerous actions to avoid urine incontinence, including:
- Maintaining a healthy weight.
- Quit smoking.
- Avoiding caffeine and alcohol.
- Practice pelvic floor exercises.
- Treating constipation quickly
- Wipe from front to back after using the restroom.
- Emptying the bladder regularly
These practices can assist in avoiding urine incontinence and lower the risk of UTIs. Furthermore, practicing safe sex with condoms can help avoid sexually transmitted diseases that can result in UTIs.
Complications and Seeking Medical Attention
If not treated, urinary incontinence can cause skin irritation, kidney infection, and sepsis. Therefore, it is critical to seek medical attention as soon as possible if one suffers symptoms of urine incontinence or UTIs, such as:
- Pain or burning sensation during urinating
- Frequent urination
- Strong urge to urinate.
- Urine that is cloudy or has a strong smell
- Blood in the Urine
Medical care is required to quickly detect and treat UTIs. Delayed treatment can result in antibiotic resistance, making treating UTIs more difficult in the future.
To summarize, implementing preventative steps and getting medical assistance promptly can help prevent urine incontinence and UTIs.
Conclusion
In conclusion, the correlation between urinary incontinence and urinary tract infections (UTIs) reveals a complex interplay that underscores the importance of holistic urinary health management. While urinary incontinence itself does not directly cause UTIs, the associated factors such as incomplete bladder emptying and frequent urinary leakage can create an environment conducive to bacterial overgrowth and infection. By understanding this relationship, individuals can take proactive steps to minimize the risk of UTIs, including practicing good hygiene, maintaining bladder health, and seeking appropriate medical interventions for urinary incontinence. Emphasizing the importance of comprehensive care and preventive measures not only alleviates the burden of recurrent UTIs but also fosters overall urinary wellness and enhances quality of life for those affected by urinary incontinence.
Trusted Health, Wellness, and Medical advice for your well-being