Health Conditions
Understanding Stage 2 Hypertension Made Easy
Are you aware of the risks of stage 2 hypertension? In this article, we will look at the complexities of this illness and help you comprehend its implications for your health.
Understanding hypertension and its stages
Hypertension, often known as high blood pressure, is a chronic disease that affects millions of individuals worldwide. It occurs when the force of blood against the walls of your arteries is consistently excessive. This disorder is known as the “silent killer” because it can go undetected for years while causing considerable damage to your cardiovascular system.
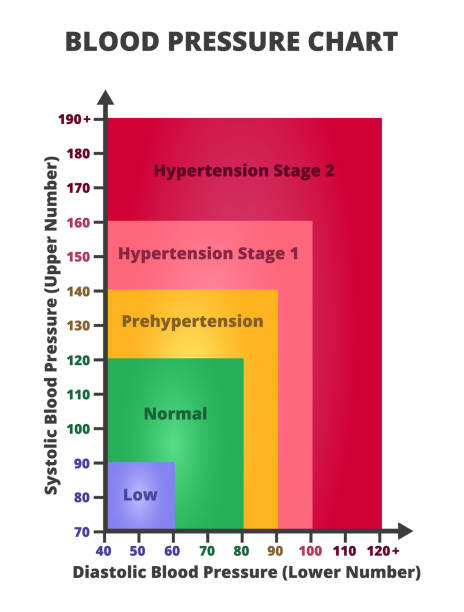
Hypertension is classified into several stages based on blood pressure readings. Stage 2 hypertension is a severe form of high blood pressure, defined by consistently elevated readings above 140/90 mmHg. These figures indicate that your heart is working harder than it should to circulate blood throughout your body, putting a significant strain on your cardiovascular system.
Causes and risk factors of stage 2 hypertension
Several causes can lead to the development of stage 2 hypertension. Some of the common causes are:
- Unhealthy lifestyle: Poor food choices, a lack of physical activity, excessive alcohol intake, and smoking can all lead to high blood pressure. These lifestyle behaviors can contribute to weight gain, high cholesterol, and poor cardiovascular health.
- Genetics and family history: Hypertension may run in families, indicating a hereditary predisposition to the ailment. If your parents or close relatives have high blood pressure, you may be more likely to have it as well.
- Age: As you age, your chances of acquiring high blood pressure increase. This is frequently due to the natural aging process, in which blood vessels become less flexible and more susceptible to plaque formation.
- Underlying medical conditions: Kidney illness, diabetes, and hormonal abnormalities can all contribute to the development of hypertension. These diseases can interfere with the regular functioning of your cardiovascular system, resulting in increased blood pressure levels.
Symptoms and signs of stage 2 hypertension
One of the challenging aspects of hypertension is that it often presents no noticeable symptoms, especially in its early stages. However, as the condition progresses to stage 2 hypertension, some individuals may experience:
- Severe headaches: High blood pressure can cause persistent, throbbing headaches. This symptom is frequently associated with dizziness and impaired vision.
- Shortness of breath: Difficulty breathing or feeling breathless even after little physical exertion can indicate stage 2 hypertension. Increased blood artery pressure can put a burden on the heart, decreasing its ability to adequately pump blood.
- Chest pain: often known as angina, occurs when the heart does not receive enough blood owing to restricted or clogged arteries. This symptom should never be disregarded, as it could indicate an approaching heart attack.
- Fatigue and weakness: Constant tiredness and a lack of energy, even after adequate rest, can indicate stage 2 hypertension. The heart must work harder to circulate blood throughout the body, which can cause weariness and weakness.
Complications associated with stage 2 hypertension
If left untreated, stage 2 hypertension can lead to severe health complications. The prolonged strain on your cardiovascular system can cause damage to blood vessels, organs, and tissues, increasing the risk of:
- Heart disease: Stage 2 hypertension considerably increases the likelihood of developing heart disease. The increased pressure within the arteries can harm the heart muscle, resulting in coronary artery disease, heart failure, and heart attacks.
- Stroke: High blood pressure is a major cause of stroke, which occurs when blood flow to the brain is disrupted. The increased pressure can cause blood vessels in the brain to burst or get clogged, creating a potentially fatal condition.
- Kidney damage: The kidneys regulate blood pressure. However, if blood pressure remains continuously high, it might cause kidney damage or even failure. This can have a significant impact on general health and well-being.
- Vision problems: Hypertension can damage the blood vessels in the eyes, causing visual issues and, in some cases, permanent vision loss. To safeguard your vision, you should take steps to control your blood pressure.

Diagnosis and medical tests for stage 2 hypertension
If you suspect you have stage 2 hypertension, it is important to consult a healthcare professional for an accurate diagnosis. Your doctor will typically perform a thorough evaluation, which may include:
- Blood pressure measurement: Your doctor will use a blood pressure cuff and a stethoscope or an automated blood pressure machine to measure your blood pressure. This will help determine if your readings consistently fall within the stage 2 hypertension range.
- Medical history and physical examination: Your doctor will ask about your medical history, lifestyle habits, and any symptoms you may be experiencing. They will also perform a physical examination to assess your overall health.
- Additional tests: Depending on your specific situation, your doctor may recommend additional tests to assess the impact of hypertension on your body. These may include blood tests, urine tests, electrocardiogram (ECG), echocardiogram, or other relevant diagnostic procedures.
Treatment options for stage 2 hypertension
Fortunately, there are several treatment options available to manage stage 2 hypertension effectively. Your doctor will develop a personalized treatment plan based on your individual needs, which may include:
- Lifestyle changes: Adopting a healthy lifestyle is essential for managing stage 2 hypertension. This involves dietary adjustments, frequent physical activity, stopping smoking, reducing alcohol use, and stress management.
- Medications: In some circumstances, lifestyle adjustments may be insufficient to regulate blood pressure. Your doctor may recommend drugs to help lower your blood pressure and lessen the likelihood of complications. These may include diuretics, beta-blockers, ACE inhibitors, calcium channel blockers, and other relevant drugs.
- Regular monitoring: It is critical to regularly measure your blood pressure and note any changes. This will allow you and your healthcare provider to analyze the efficacy of your treatment plan and make any required changes.
Lifestyle changes to manage stage 2 hypertension
In addition to medical interventions, there are several lifestyle changes you can make to effectively manage stage 2 hypertension:
- Dietary changes: Eat a heart-healthy diet rich in lean meats, whole grains, fruits, vegetables, and low-fat dairy. Limit your consumption of sodium, saturated fat, and cholesterol.
- Regular exercise: Regular exercise is engaging in moderate-intensity physical activity for at least 150 minutes per week. This can include brisk walking, cycling, swimming, or any other type of exercise that raises your heart rate.
- Weight management: If you are overweight or obese, lowering even a small amount of weight will significantly lower your blood pressure. Aim for a healthy weight range by combining nutrition and activity.
- Stress management: Find healthy strategies to cope with stress, as persistent stress can lead to high blood pressure. Deep breathing exercises, meditation, yoga, or indulging in enjoyable hobbies can all help you relax.
- Limit your alcohol consumption and quit smoking: Both alcohol and smoking can lead to high blood pressure. To improve your cardiovascular health, limit your alcohol use and consider stopping smoking entirely.

Prevention and reducing the risk of stage 2 hypertension
While some risk factors for stage 2 hypertension, such as age and genetics, are beyond our control, there are steps we can take to reduce the risk and prevent the condition from worsening:
- Regular blood pressure checks: Regular blood pressure readings can help identify changes and allow for early action if necessary. This is especially crucial if your family history includes high blood pressure or other risk factors.
- Healthy lifestyle habits: Healthy habits, such as eating a balanced diet, exercising regularly, and managing stress, can dramatically lower the chance of having stage 2 hypertension. It’s never too late to improve your health.
- Manage underlying health concerns: If you have diabetes or kidney disease, consult with your doctor to determine how to best treat these conditions. This allows you to limit the effect they may have on your blood pressure.
- Regular medical check-ups: Make regular appointments with your healthcare practitioner to maintain your overall health and identify any potential risk factors. Regular screenings and early management can assist to slow the progression of hypertension.
Conclusion
Stage 2 hypertension is a serious medical condition that demands immediate attention and suitable treatment. Understanding the origins, symptoms, problems, and treatment options will allow you to manage your blood pressure and protect your health.
Remember that managing stage 2 hypertension requires a combination of lifestyle changes, medication therapies, and regular monitoring. You can effectively manage stage 2 hypertension and limit its effects on your well-being by maintaining a healthy lifestyle, working closely with your healthcare practitioner, and sticking to your treatment plan.
Don’t wait for symptoms or consequences to develop. Take proactive steps to improve your cardiovascular health and enjoy a healthy future.
Trusted Health, Wellness, and Medical advice for your well-being


