Alternative Treatments, Health Conditions
What are the Treatment Options for Blocked Arteries in Your Neck?
The primary goal of knowing the treatment options for blocked arteries in your neck is to reduce the risk of stroke, which can be disabling and even fatal. The treatment options are diverse and personalized to each individual’s unique circumstances, taking into account the degree of artery blockage, the presence of concomitant symptoms, the patient’s age, and overall health profile.
The diagnosis of blocked arteries in the neck, known as carotid artery disease, can be overwhelming. With the prospect of stroke approaching, recognizing the available treatment choices is critical. Navigating the therapeutic spectrum, from lifestyle changes to surgical procedures, necessitates an understanding of the condition’s complexities and tailored care techniques.
In this article, we will look at the many treatment options available for managing blocked arteries in the neck, throwing light on the most recent advances and guiding principles in vascular health. Whether you’re a patient looking for answers or a healthcare professional looking for new treatment options, join us on this journey to discover the broad panorama of interventions meant to protect against blocked arteries.

Lifestyle Changes
The severity of carotid artery blockage serves as a pivotal determinant in guiding treatment decisions. Mild to moderate blockages may necessitate lifestyle modifications and medication management aimed at stabilizing plaque buildup and reducing the risk of clot formation.
Lifestyle changes emerge as a key component of treatment, providing a proactive strategy to slowing the formation of fatty deposits and lowering the risk of stroke. Embracing a healthier lifestyle entails a variety of adjustments that have a significant impact on vascular health.
Quitting Smoking
This is one of the most important measures towards reducing the harmful effects of carotid artery disease. Cessation not only reduces the introduction of dangerous substances into the bloodstream, but it also encourages the slow reversal of arterial damage, creating an environment conducive to healing and restoration.
Weight Management
This is also important, as excess body weight contributes to arterial plaque production and systemic inflammation. Individuals can engage on a path to lose weight and reduce the strain on their cardiovascular system by making attentive eating choices and controlling their portion sizes.
Adopting a Nutrient-dense Diet
This is central to this paradigm change. Individuals can improve their cholesterol levels, blood pressure, and overall metabolic health by prioritizing these nutritious foods and reducing their consumption of processed and high-sodium foods.
Regular Physical Activity
This appears as a key component in the pursuit of vascular well-being. Aerobic activity, such as brisk walking, swimming, or cycling, not only improves cardiovascular fitness but also stimulates arterial dilatation, increases blood flow, and strengthens the body’s ability to fight vascular illness.
In summary, lifestyle modifications act as a powerful tool in the fight against carotid artery disease, allowing people to take charge of their health and pave the road to longevity and vitality. By implementing these holistic treatment measures, one can not only prevent the growth of blocked arteries but also cultivate a foundation of well-being that extends beyond vascular health.
Medication
Medications play a pivotal role in controlling and mitigating the risk factors that underpin carotid artery disease. Through targeted pharmacotherapy, healthcare providers aim to address key contributors to arterial plaque formation and vascular dysfunction, thereby reducing the likelihood of stroke and enhancing overall cardiovascular health.

Anti-hypertensive Drugs
High blood pressure, a prevalent precursor to carotid artery disease, often necessitates intervention with antihypertensive medications. These drugs work to normalize blood pressure levels, alleviating the strain on arterial walls and mitigating the risk of plaque rupture or thrombosis. By optimizing blood pressure control, individuals can safeguard against the progression of arterial blockages and minimize the occurrence of cardiovascular events.
In addition to your age, race, and gender/sex, your healthcare practitioner will examine your other health issues and blood pressure level when determining which high blood pressure medicine to prescribe. Your treatment will differ from your neighbor’s or brother’s medications because every one of you has a unique condition.
To lower your blood pressure, you may need to take multiple types of high blood pressure medications. Your doctor may start with one antihypertensive medication and gradually add another or three. They may also initiate and discontinue antihypertensive medications if they do not produce results or if you have unbearable side effects or hazardous changes in your bloodwork. Your healthcare physician will most likely ask you to take your blood pressure at home each morning before you consume any coffee.
Most individuals take blood pressure medications in the form of pills that they swallow every day, however, your doctor may administer antihypertensive medications through an IV (intravenous) in your arm during a hospitalization.
Examples of anti-hypertensive drugs:
Some of the more regularly recommended medications for hypertension include:
Diuretics or Water Tablets
These are frequently the first medications used to treat essential hypertension; examples include hydrochlorothiazide, thiazide, indapamide, and chlorthalidone. As the name implies, these medications act on the kidneys to increase the quantity of water excreted in the urine, lowering the blood volume inside the body and hence the blood pressure.
Furthermore, certain diuretics dilate or relax the walls of the arteries, allowing blood to flow more easily through these channels and thereby lowering blood pressure.
Selected blood pressure medication side effects:
- Magnesium and potassium levels can be either high or low.
- An upset stomach.
- High uric acid levels.
- Dizziness.
Adrenergic blockers (including alpha, beta, alpha-beta, and peripherally acting blockers)
Beta-blockers include atenolol, metoprolol, nadolol, pindolol, carvedilol, and labetelol. These drugs block the heart’s beta receptors, lowering the force with which the heart pumps. Beta-blockers also reduce the heart rate.
Alpha Blockers
These work by inhibiting the alpha-adrenergic receptors, which relax and widen blood vessels. This lowers the pressure against which the heart must pump, and hence the blood pressure.
Selected blood pressure medication side effects:
- Fainting.
- Dizziness.
- Tiredness.
- Low heart rate.
Calcium Channel Blockers
These drugs prevent calcium from flowing through the blood vessel muscles, causing them to relax and dilate. This lowers the pressure against which the heart must pump, and hence the blood pressure. These agents include amlodipine, nifedipine, nicardipine, and verapamil.
Selected blood pressure medication side effects:
- Headache.
- Dizziness.
- Fast or slow heart rate.
- Lower leg swelling.
Angiotensin-converting enzyme (ACE) inhibitors
These medications inhibit the activity of angiotensin II, which typically constricts blood arteries. Blocking its activity dilates blood arteries, lowering blood pressure. Examples of these agents are enalapril, captopril, and ramipril.
Selected blood pressure medication side effects:
- Cough.
- High potassium.
- Dizziness.
- Angioedema (swelling of the face and neck); if you experience this serious reaction, do not take an ACE inhibitor again.
Centrally Acting Sympatholytics
These are chemicals that work on the central nervous system to cause blood vessel dilatation and, consequently, blood pressure. This class of drugs includes clonidine and methyldopa. Methyldopa is appropriate for pregnant women who have hypertension.
Selected blood pressure medication side effects:
- Tiredness.
- Dry mouth.
- Slow heart rate.
Vasodilators
This class of drugs includes hydralazine and minoxidil, which relax the smooth muscle of blood arteries, leading them to relax and widen. Again, this lessens the pressure against which the heart must pump, and therefore lowers blood pressure.
Selected blood pressure medication side effects:
- Rapid heart rate.
- Headache.
- Lower leg edema.

Statins
Similarly, elevated cholesterol levels represent a modifiable risk factor for carotid artery disease, warranting treatment with lipid-lowering agents such as statins. By inhibiting the production of cholesterol and promoting its clearance from the bloodstream, statins serve as frontline defenders against atherosclerosis, the underlying pathology driving arterial narrowing and stenosis. Through sustained adherence to statin therapy, individuals can not only attenuate plaque accumulation but also foster plaque stability, reducing the propensity for rupture and embolization.
Here are the commonly prescribed statins:
- Atorvastatin (Lipitor).
- Fluvastin (Lescol XL).
- Lovastatin (Altoprev).
- Pitavastatin (Livalo).
- Pravastatin.
- Rosuvastatin (Crestor).
- Simvastatin (Zocor).

Anticoagulants
Blood thinners, or anticoagulants, constitute another cornerstone of medical management for carotid artery disease, particularly in cases where individuals are at heightened risk of thromboembolic events. These agents impede the formation of blood clots within narrowed arterial segments, mitigating the likelihood of clot dislodgement and subsequent cerebral infarction.
By promoting antithrombotic effects, blood thinners serve as a critical adjunct to traditional therapies, bolstering the efficacy of interventions aimed at preserving cerebral perfusion and averting stroke.
The most often prescribed anticoagulant is warfarin.
Newer anticoagulants are also available and becoming more frequent. This includes:
- Rivaroxaban (Xarelto)
- Dabigatran (Pradaxa)
- Apixaban (Eliquis)
- Edoxaban (Lixiana)
Warfarin and its newer substitutes are administered as tablets or capsules. Heparin, another type of anticoagulant, can also be administered via injection.
Other Treatment Alternatives: Surgery
Surgery for carotid artery disease seeks to restore normal blood flow to the brain by removing or bypassing the blockage. Various surgical procedures may be used, each with its own set of benefits and hazards. From carotid endarterectomy to carotid artery stenting, these operations provide feasible options for people with significant arterial blockages who are in danger of having a debilitating stroke.
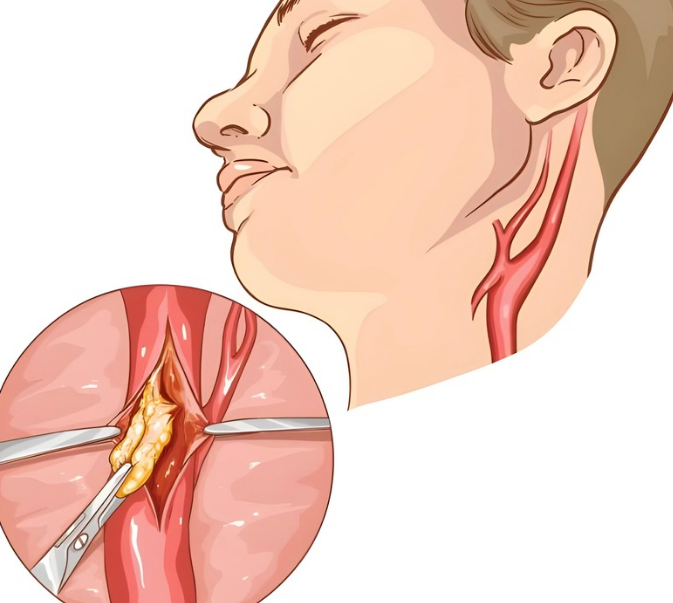
Carotid Endarterectomy
Carotid endarterectomy (CEA) is a cornerstone in the treatment of carotid atherosclerosis, especially for people who have had transient ischemic episodes (TIAs) or small strokes. CEA, which is well-known for its ability to reduce the incidence of repeated cerebrovascular episodes, provides a final option for restoring cerebral perfusion and avoiding stroke.
What happens in this procedure?
Under general anesthesia, the surgical procedure begins with a precise incision in the neck at the point of artery occlusion. The surgeon moves with great precision through the layers of tissue to expose the carotid artery, laying the groundwork for the revolutionary movements that will follow.
The surgeon carefully separates the damaged part of the artery, negotiating the complex terrain of vascular anatomy with surgical dexterity. The obstructive plaque is carefully removed using specialized instruments and procedures, freeing the arterial conduit from the shackles of stenosis and ushering in a new era of uninterrupted blood flow to the brain.
The complicated technique culminates in the precise closure of the carotid artery, which ensures hemostasis and structural integrity. The artery is flawlessly rejoined using precision suturing procedures, ushering in an age of improved vascular patency and lower stroke risk.
However, deciding to have CEA requires thorough consideration of the associated risks and benefits, with critical parameters such as age, degree of artery blockage, and prior cerebrovascular episodes determining the treatment paradigm. While CEA has unquestionable benefits in lowering the incidence of stroke recurrence, it is not without risks, including surgical site infection, nerve injury, and perioperative stroke.
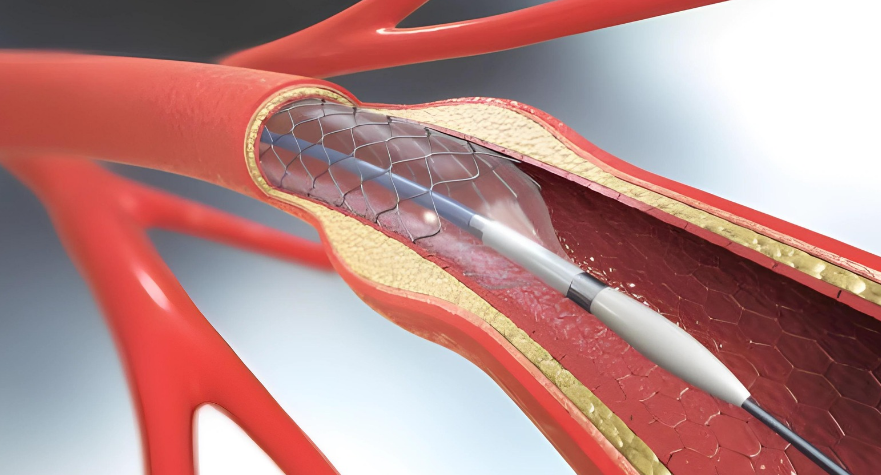
Carotid Artery Stenting
Carotid artery stenting (CAS) is a cutting-edge therapeutic option for carotid artery disease, giving a less invasive method than standard carotid endarterectomy. Conducted in a catheterization laboratory, CAS exemplifies the junction of technological progress and clinical experience, offering consumers a feasible option for lowering the risk of stroke and restoring vascular health.
What happens in this procedure?
The procedure begins with a small puncture in the groin area, which serves as the entrance to the arterial highway. Through this access site, a specially constructed catheter travels to the epicenter of vascular disease, guided by modern imaging modalities and expert interventionalists.
When the catheter reaches the target point of artery constriction, it unleashes its transforming power by delivering a small balloon tip that is precisely inflated for a brief period. This transient expansion acts as a stimulant for arterial dilation, much like coaxing open the gates of a fortress besieged by advancing plaque.
A stent—a slender tube similar to a scaffold—is surgically positioned within the artery conduit, poised to maintain vascular integrity and reinforce the walls against illness. The stent, made of robust metals or bioabsorbable materials, takes on a permanent or transient presence within the artery, acting as a beacon of hope in the fight against repeated stenosis and thromboembolic events.
Despite the potential inherent in CAS, its introduction has resulted in a convergence of viewpoints and conflicts over its comparative efficacy and safety to traditional CEA. While current data suggests that CEA may have a modestly decreased risk of post-procedural stroke or mortality, the landscape of vascular therapies is dynamic and constantly evolving.
Thus, the decision to pursue CAS needs a nuanced assessment of personal risk profiles and treatment objectives, which is supported by informed consent and collaborative decision-making. By leveraging the collective experience of doctors, researchers, and patients, we may traverse the complexity of carotid artery disease with caution and discernment, paving the way for optimal vascular outcomes and enhanced quality of life.
Disclaimer: Please note that Discoverybody has taken great care to ensure that all information provided is comprehensive and up-to-date. However, you should not use this article as a substitute for the expertise that a licensed healthcare professional can offer. It’s always a good idea to talk to your doctor before taking any medication.
Sources Expanded
Torborg, L. (2018, November 30). Mayo Clinic Q and A: New treatment to open blocked carotid artery. Mayo Clinic News Network. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-new-treatment-to-open-blocked-carotid-artery/
Medical treatments for carotid artery disease. (2017, September 11). Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/carotid-artery-disease/treatments/medical.html#:~:text=Medications,are%20examples%20of%20antiplatelet%20medications.
Professional, C. C. M. (n.d.). Blood Pressure Medication. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/21811-antihypertensives
Website, N. (2022, May 17). Anticoagulant medicines. nhs.uk. https://www.nhs.uk/conditions/anticoagulants/
Carotid artery disease – Diagnosis and treatment – Mayo Clinic. (2023, April 19). https://www.mayoclinic.org/diseases-conditions/carotid-artery-disease/diagnosis-treatment/drc-20360527
Samson, M. (n.d.). Hypertension Medication: Diuretics, Thiazide, Diuretic, Potassium-Sparing, Diuretics, Loop, ACEIs, ARBs, Beta-Blockers, Beta-1 Selective, Beta-Blockers, Alpha Activity, Beta-Blockers, Intrinsic Sympathomimetic, Vasodilators, Calcium Channel Blockers, Aldosterone Antagonists, Selective, Alpha2-agonists, Central-acting, Renin Inhibitors/Combos, Alpha-Blockers, Antihypertensives, Antihypertensives, Other, Antihypertensive Combinations. https://emedicine.medscape.com/article/241381-medication?form=fpf
Trusted Health, Wellness, and Medical advice for your well-being



